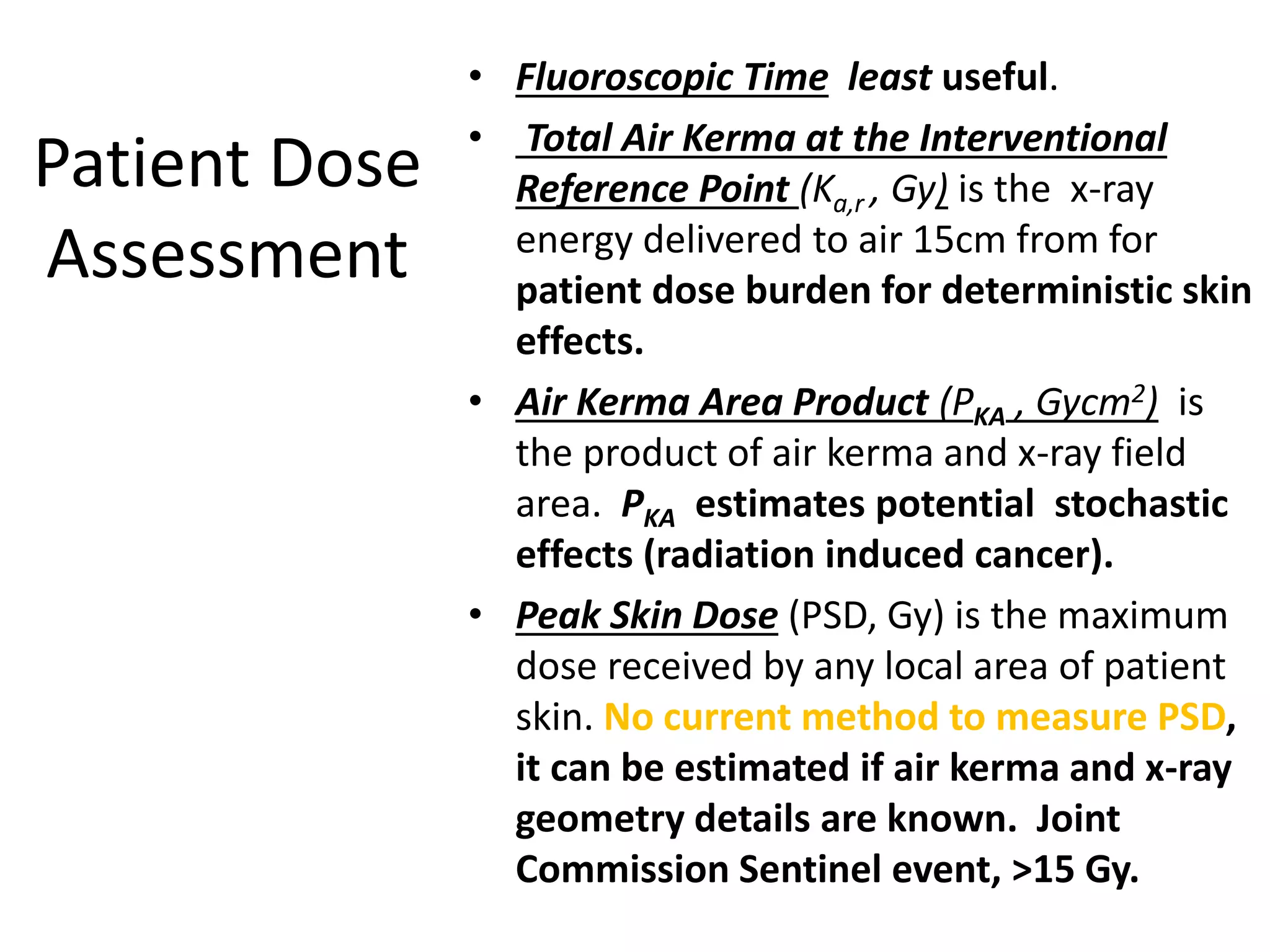
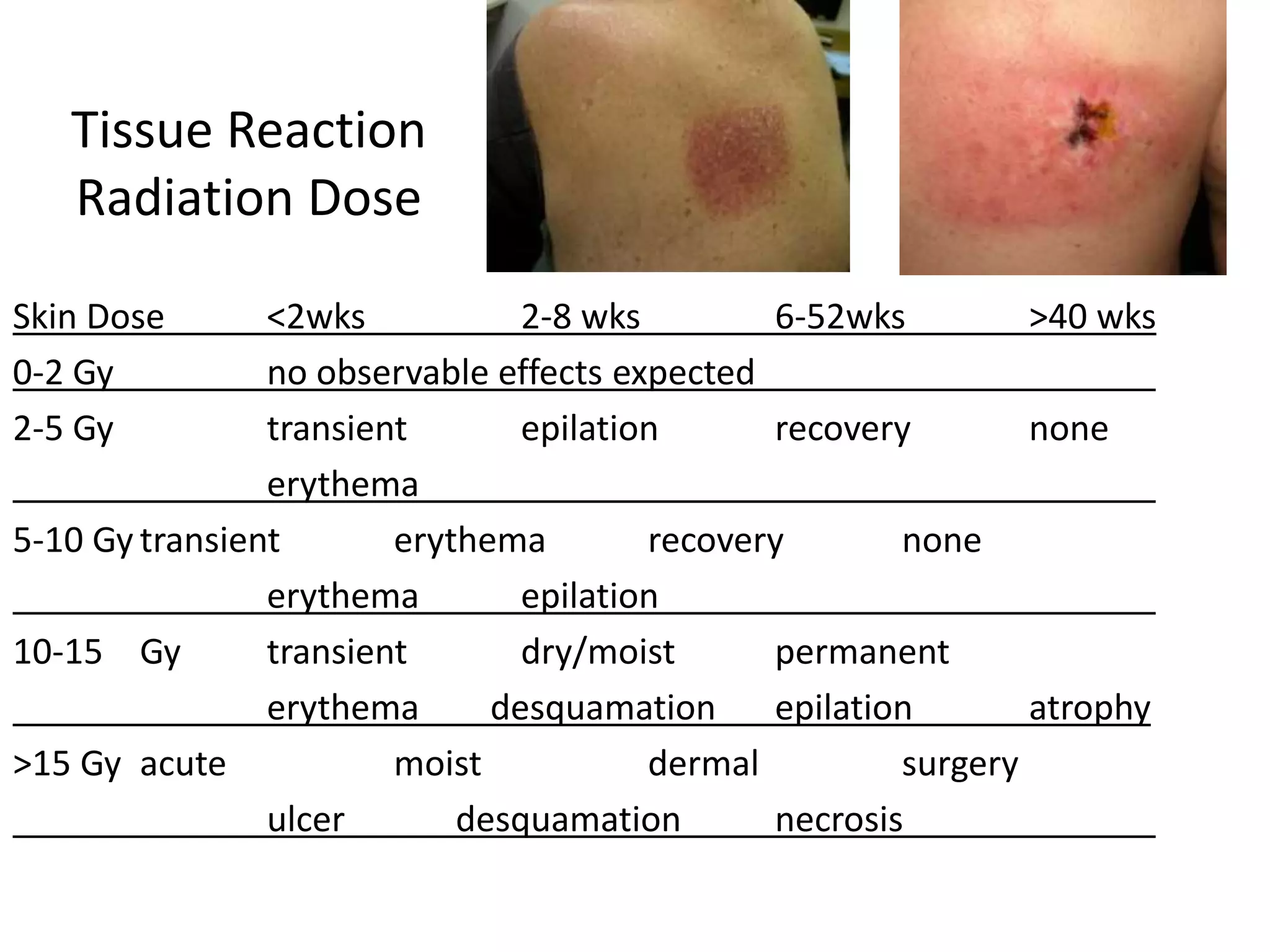
This document discusses radiation safety in cath labs. It explains that increasing mA increases radiation exposure while increasing kVp decreases absorption. Fluoroscopy requires less radiation than cineangiography. Key metrics for measuring patient radiation dose include fluoroscopic time, air kerma, and peak skin dose. Both stochastic effects like cancer and deterministic effects like skin burns are risks. Proper techniques like limiting fluoro use, collimation, and distancing can reduce radiation exposure for patients and staff. New technologies also aim to improve radiation protection.