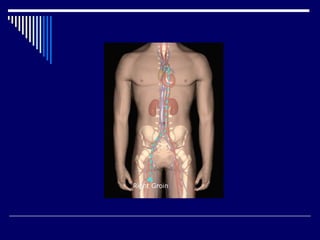
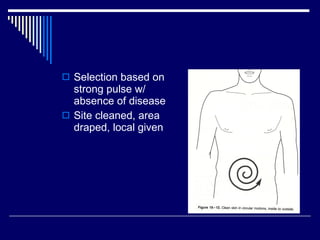
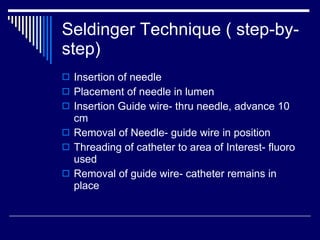
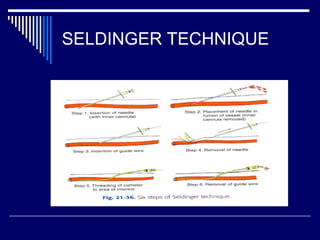
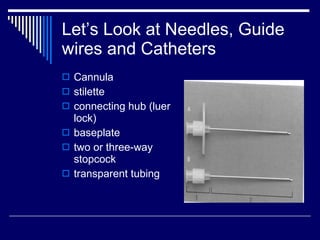
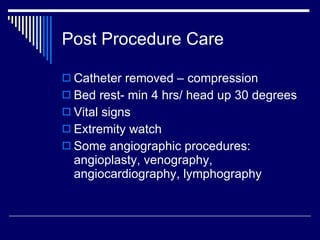
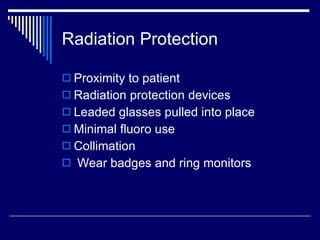
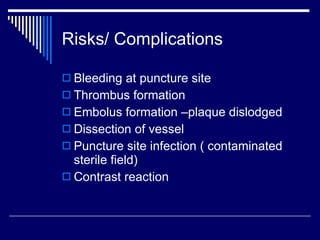
The document discusses angiography procedures and equipment. It describes the personnel involved including radiologists, nurses, and technologists. It outlines the angiography room setup and various equipment used, including x-ray generators, tubes, injectors, and digital imaging systems. Key steps of the Seldinger technique for vascular catheter insertion are provided. Post-procedure care and risks are also summarized.