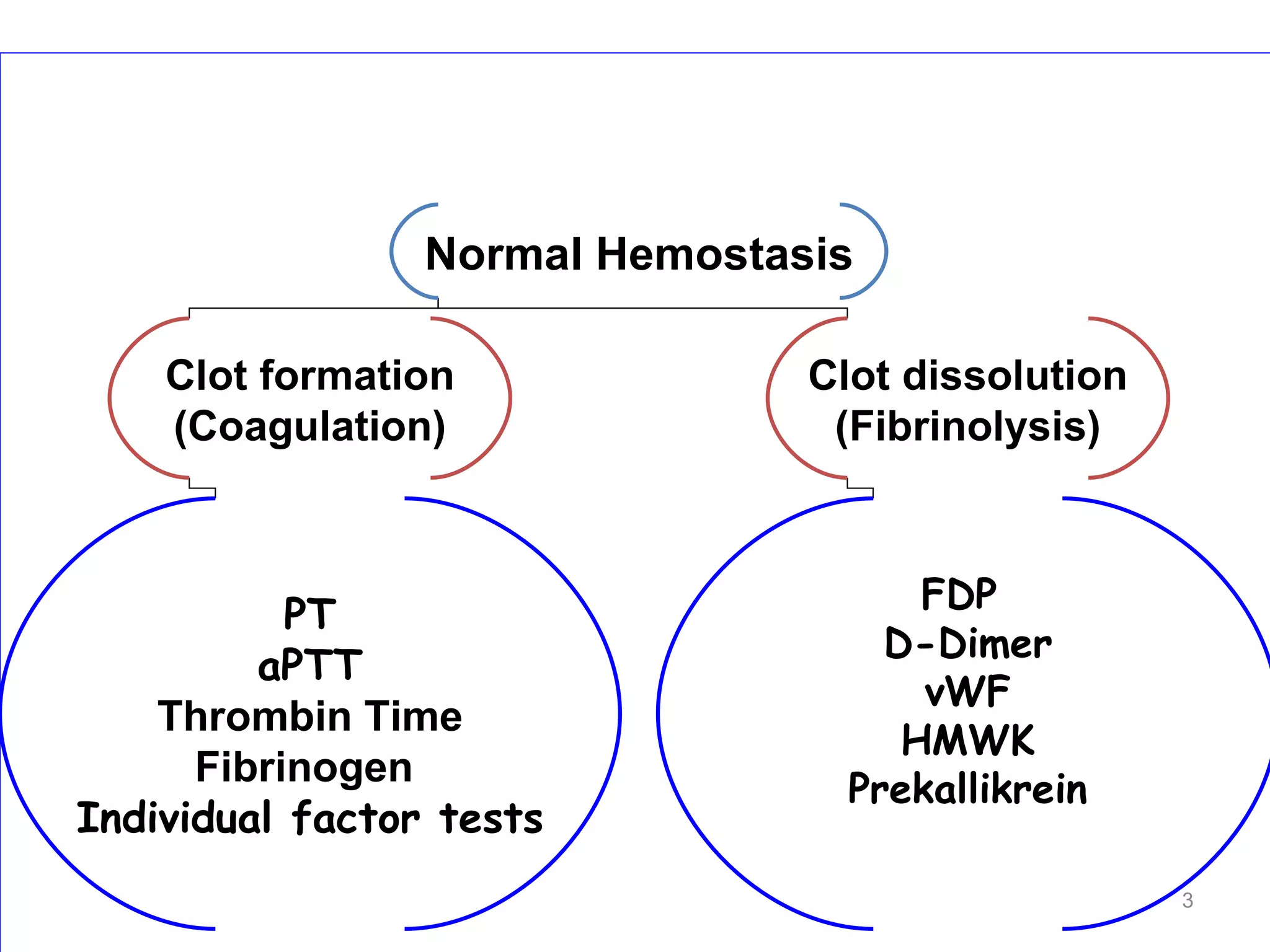
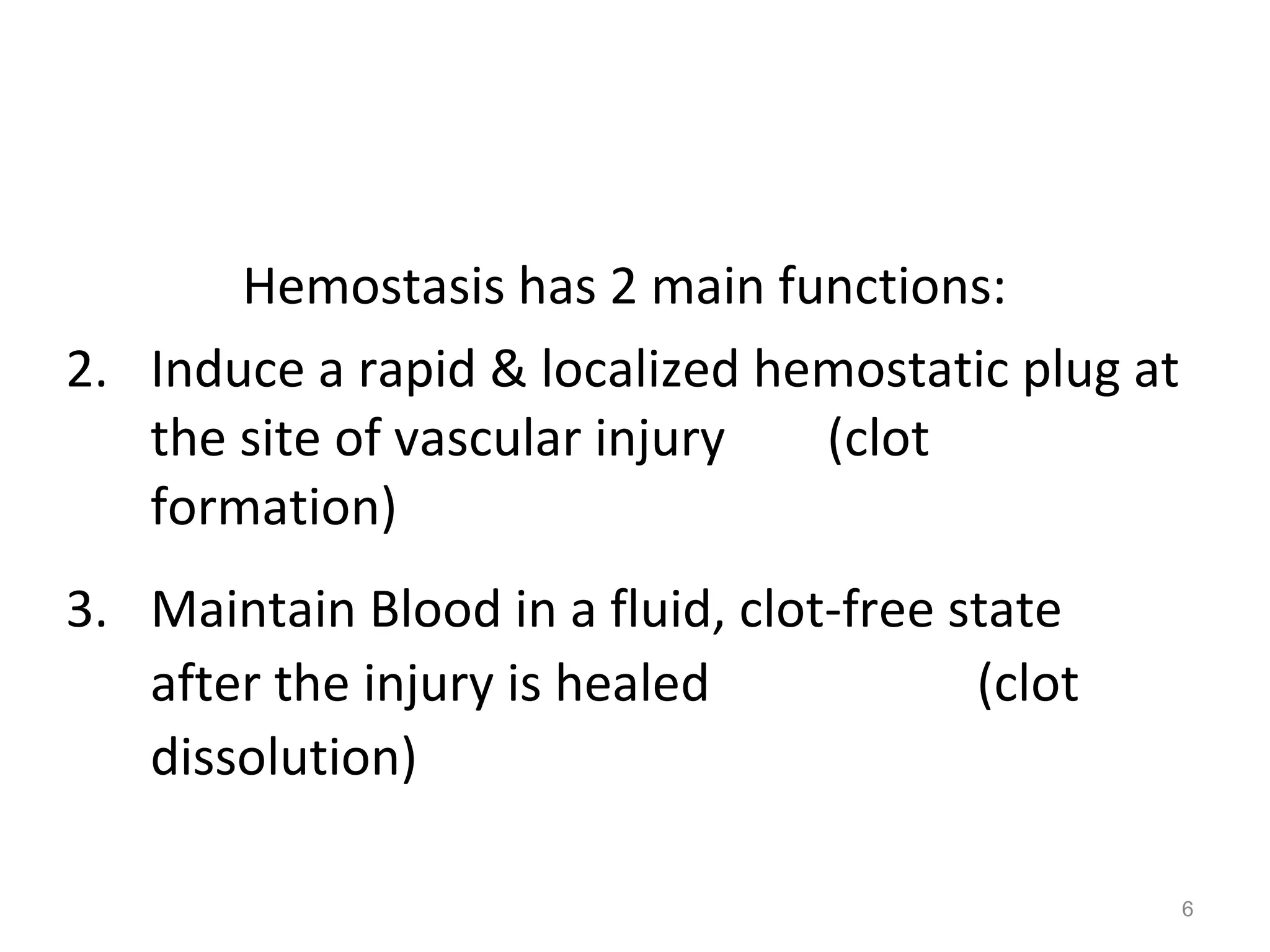
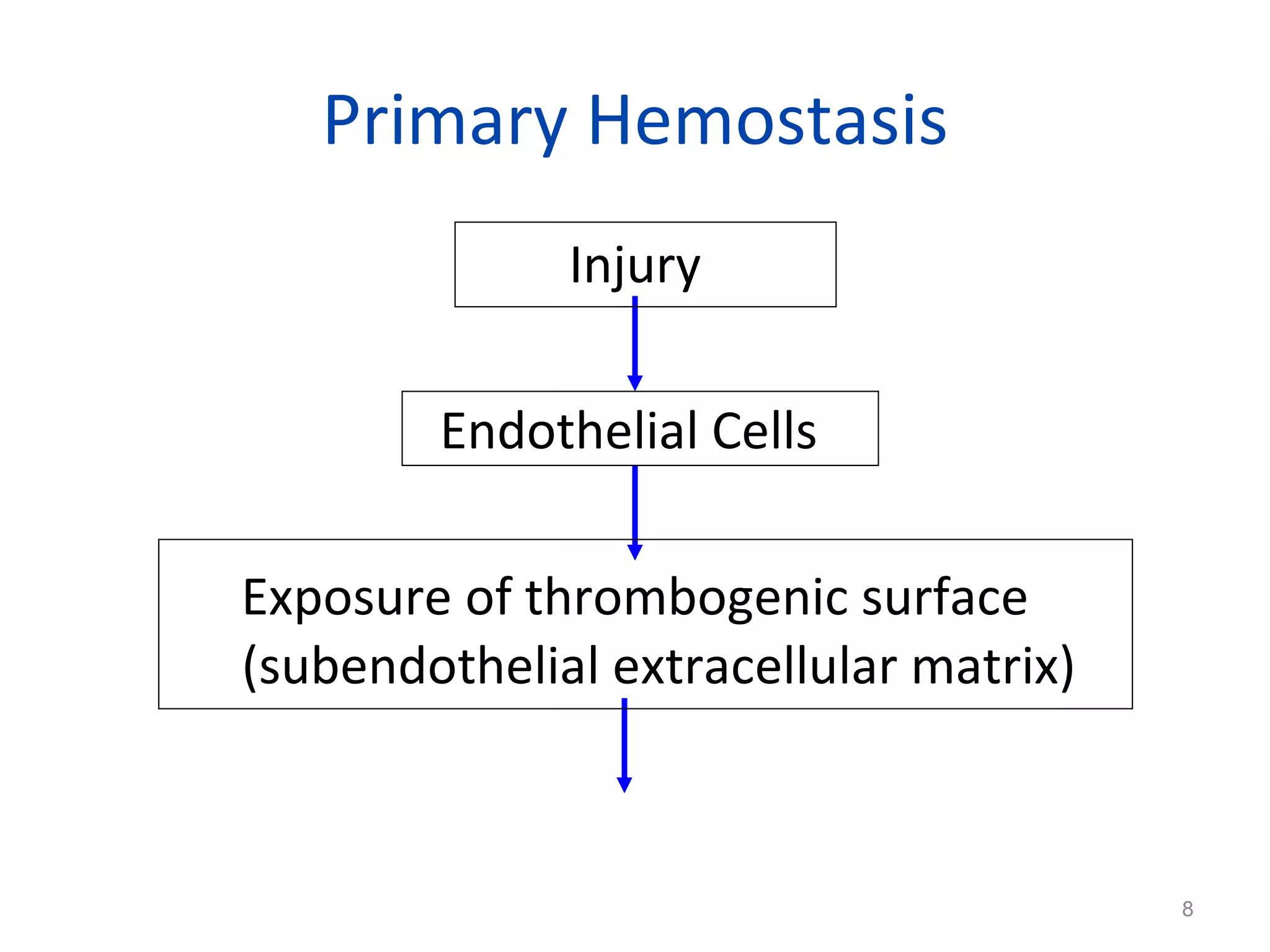
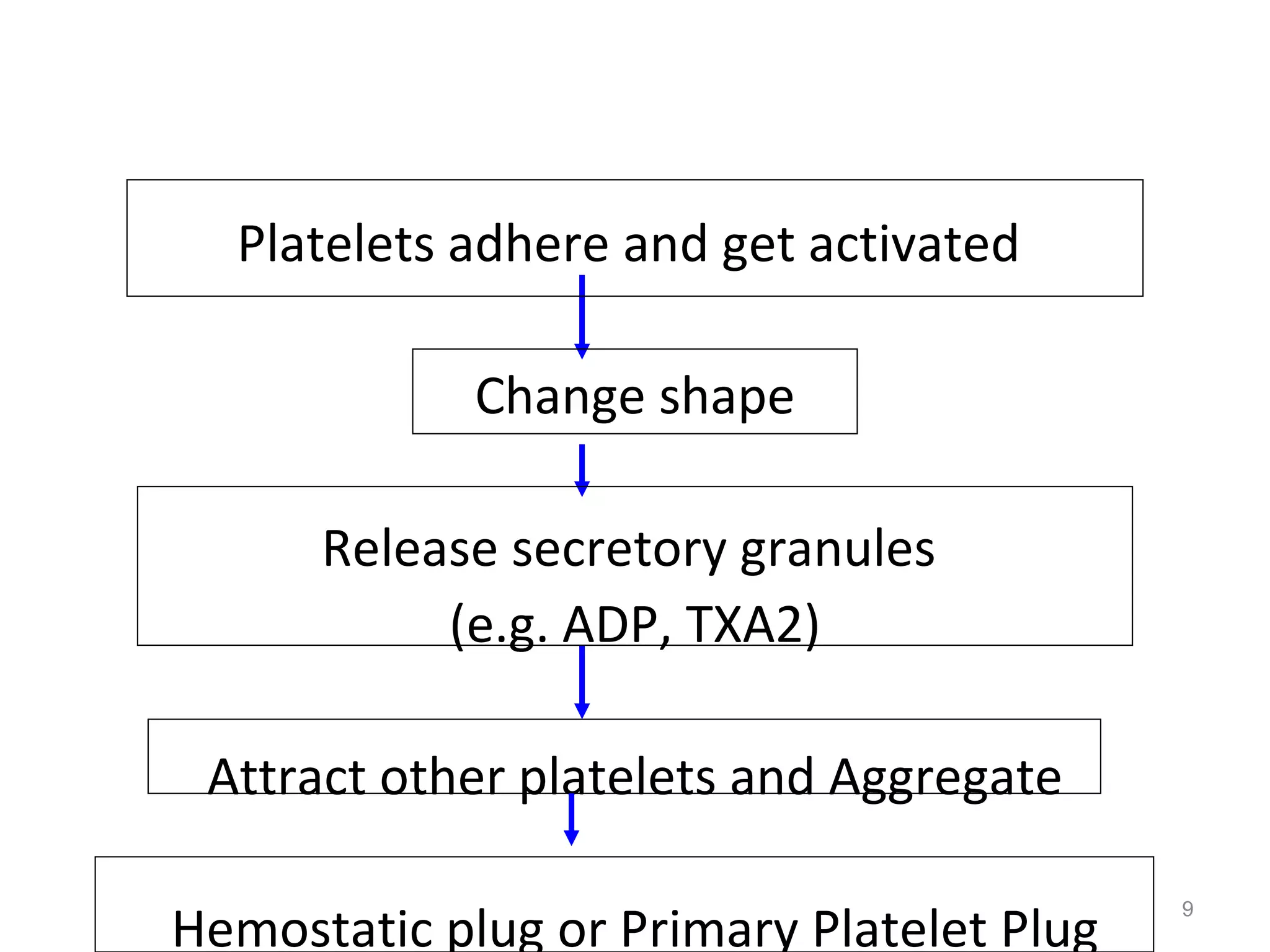
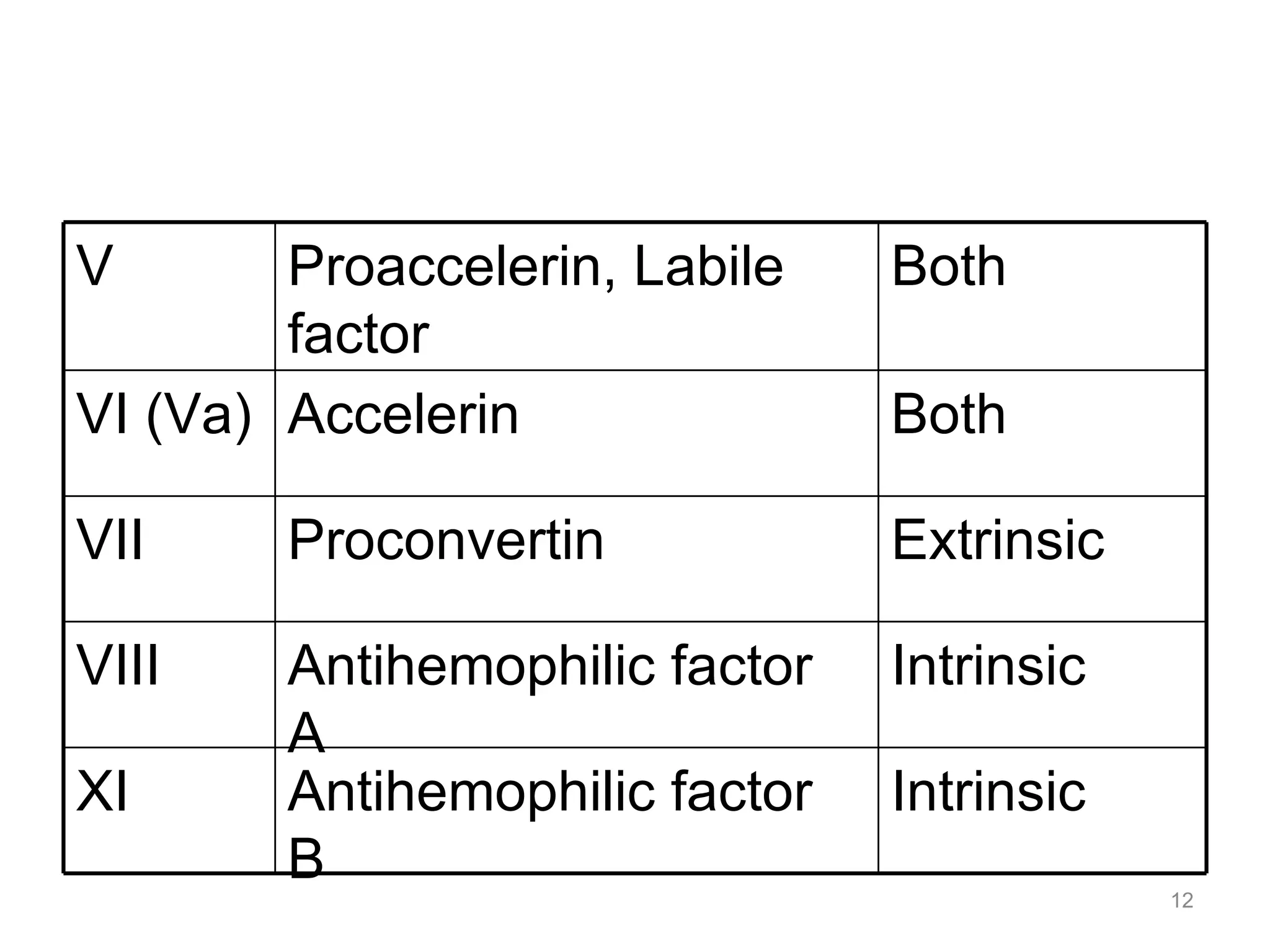
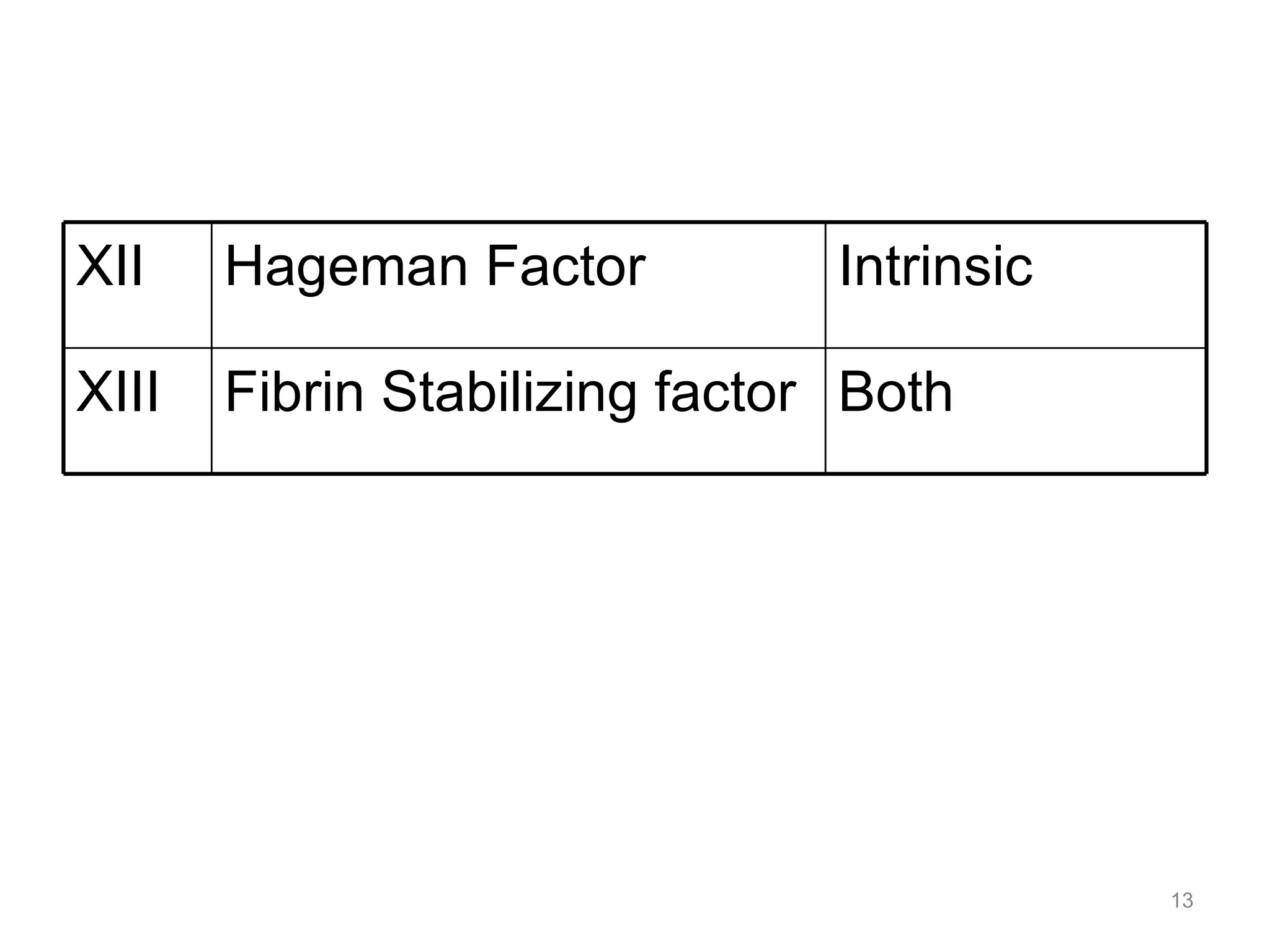
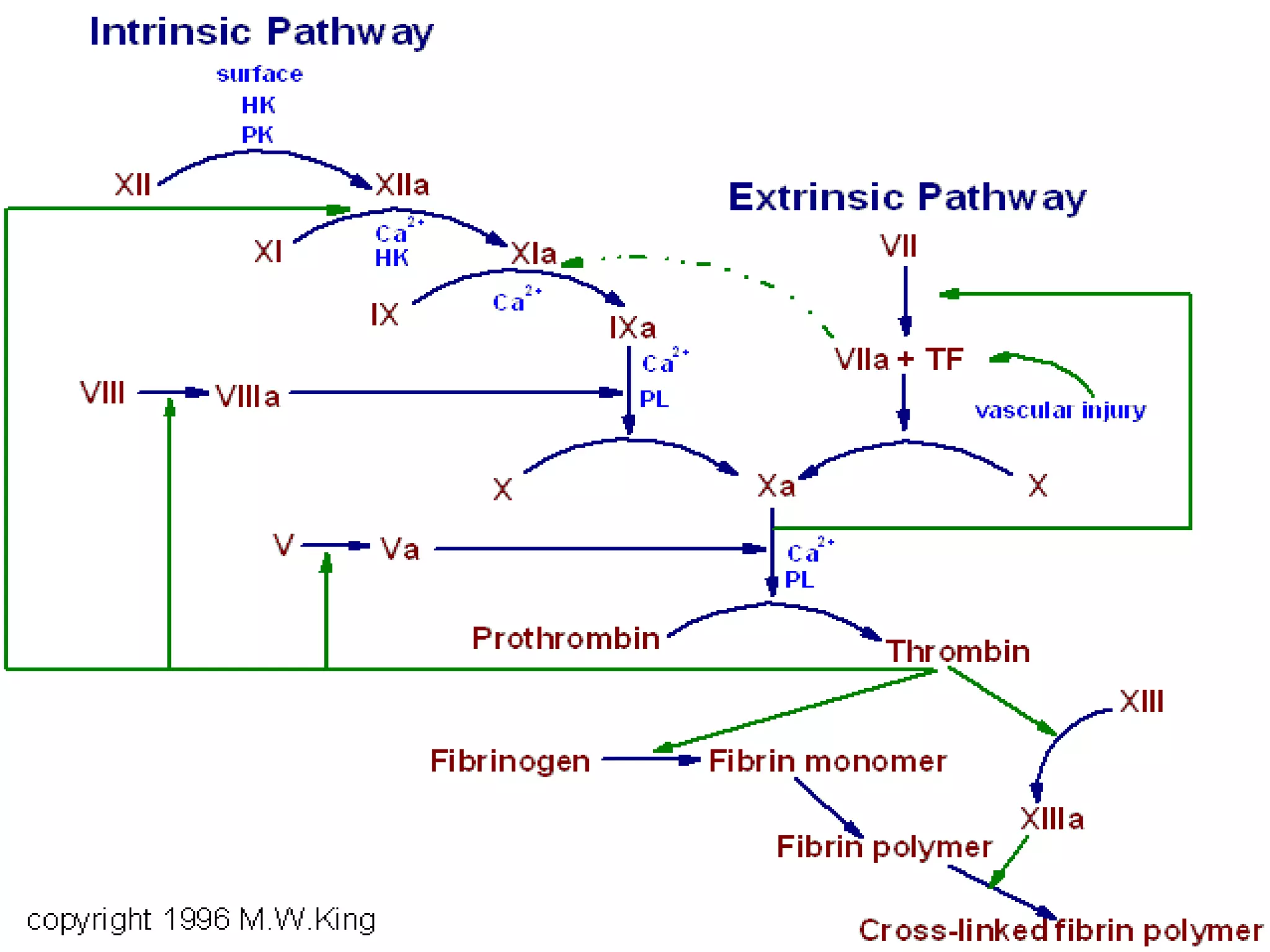
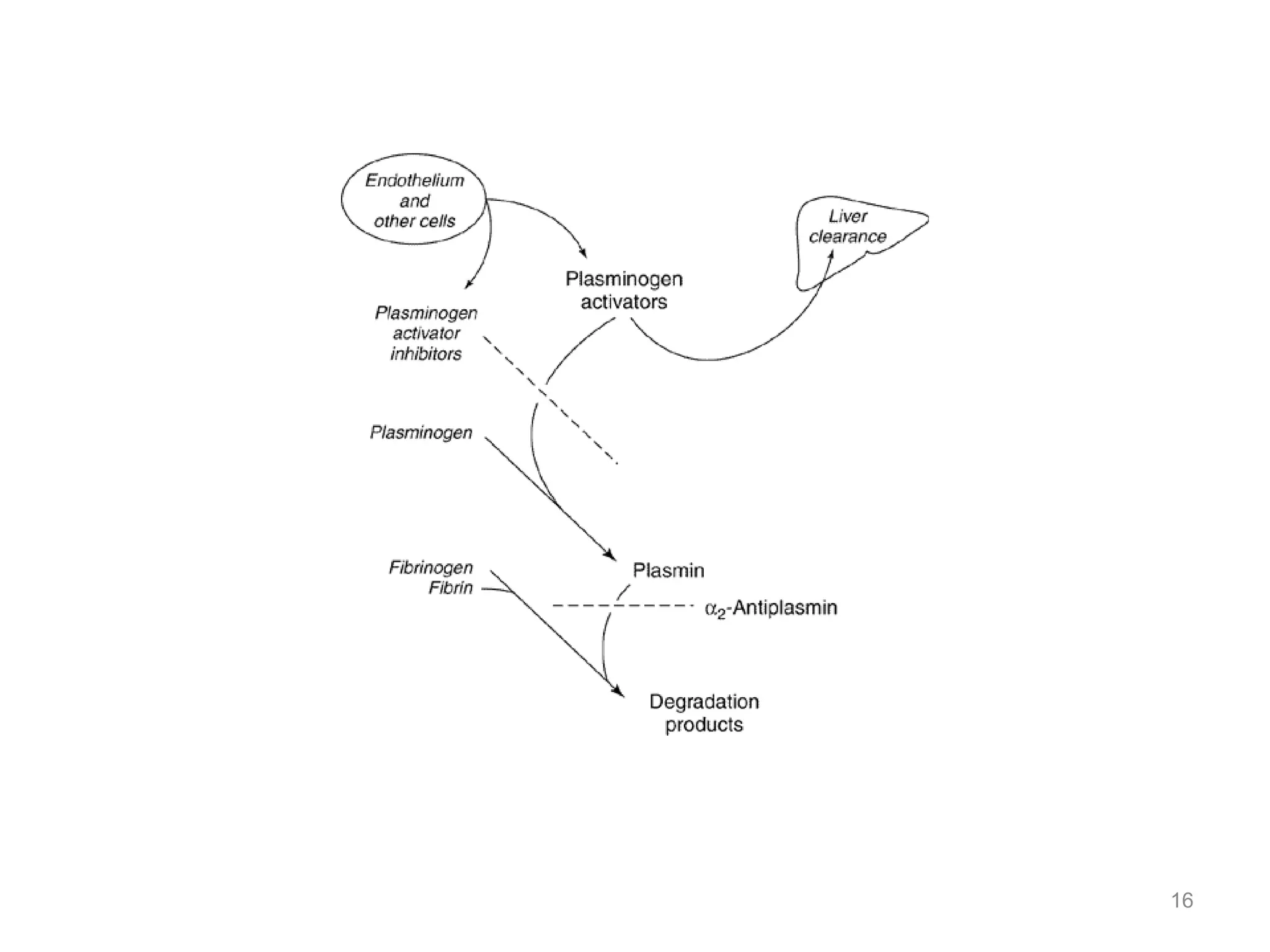
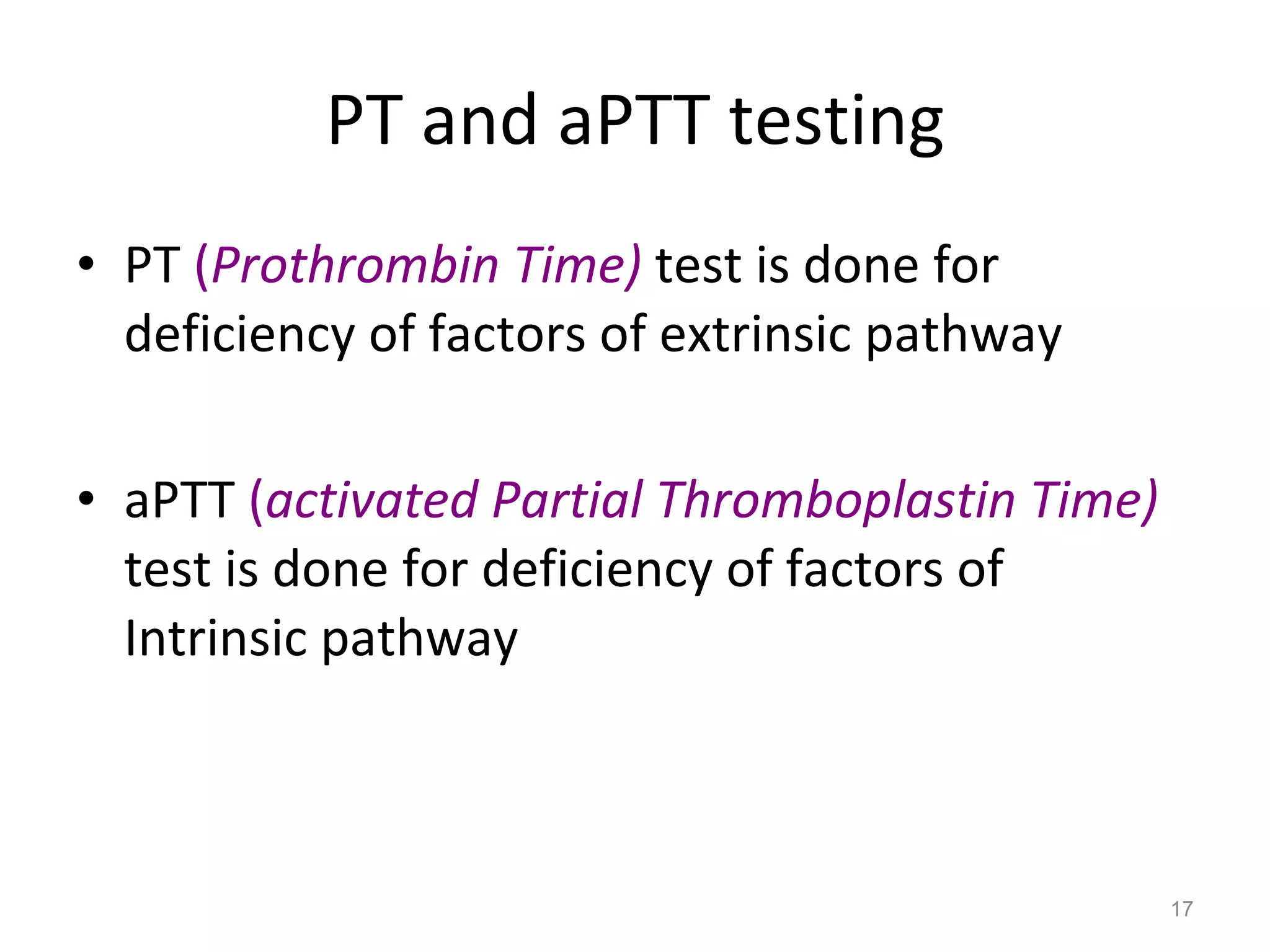
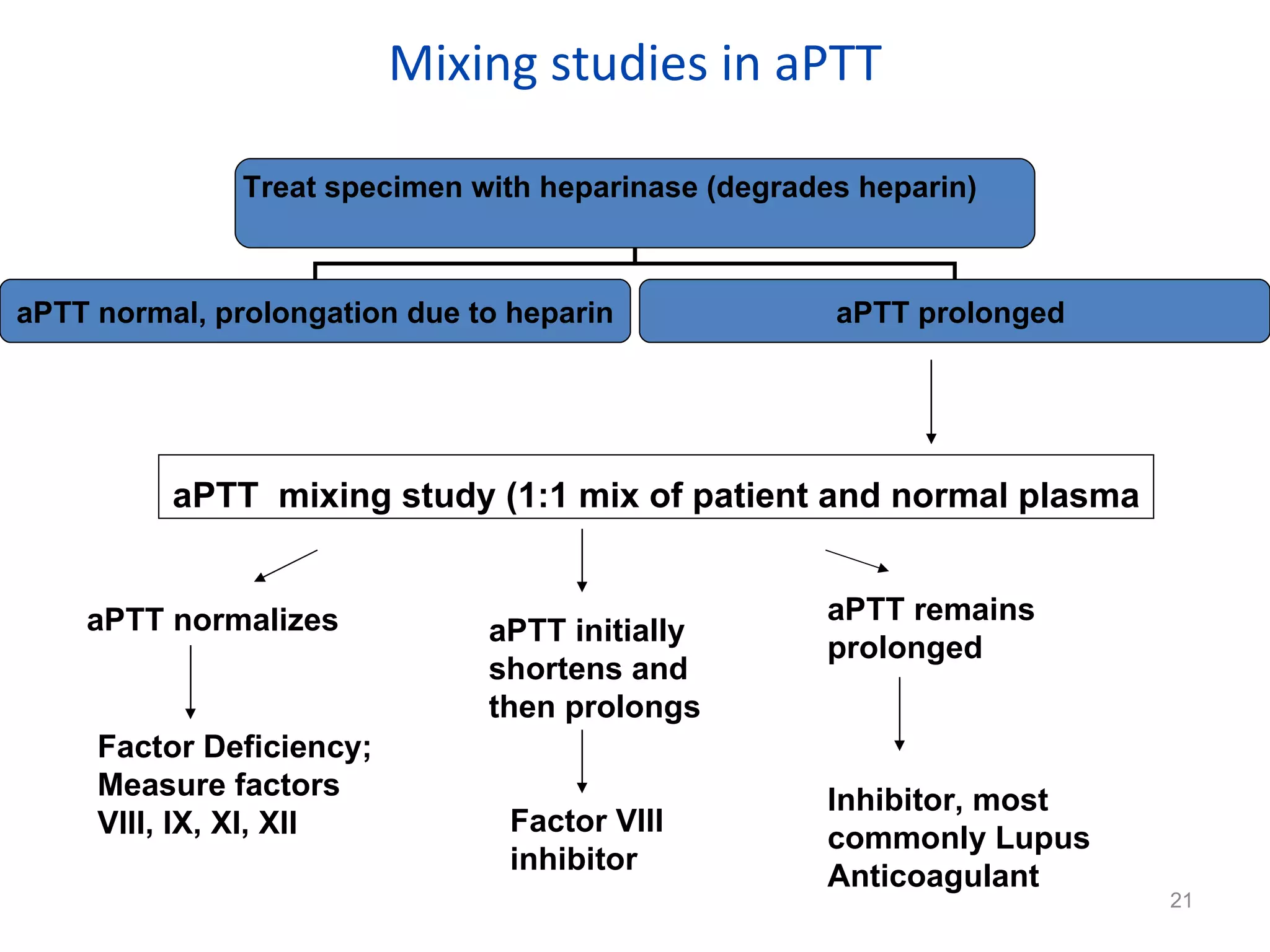
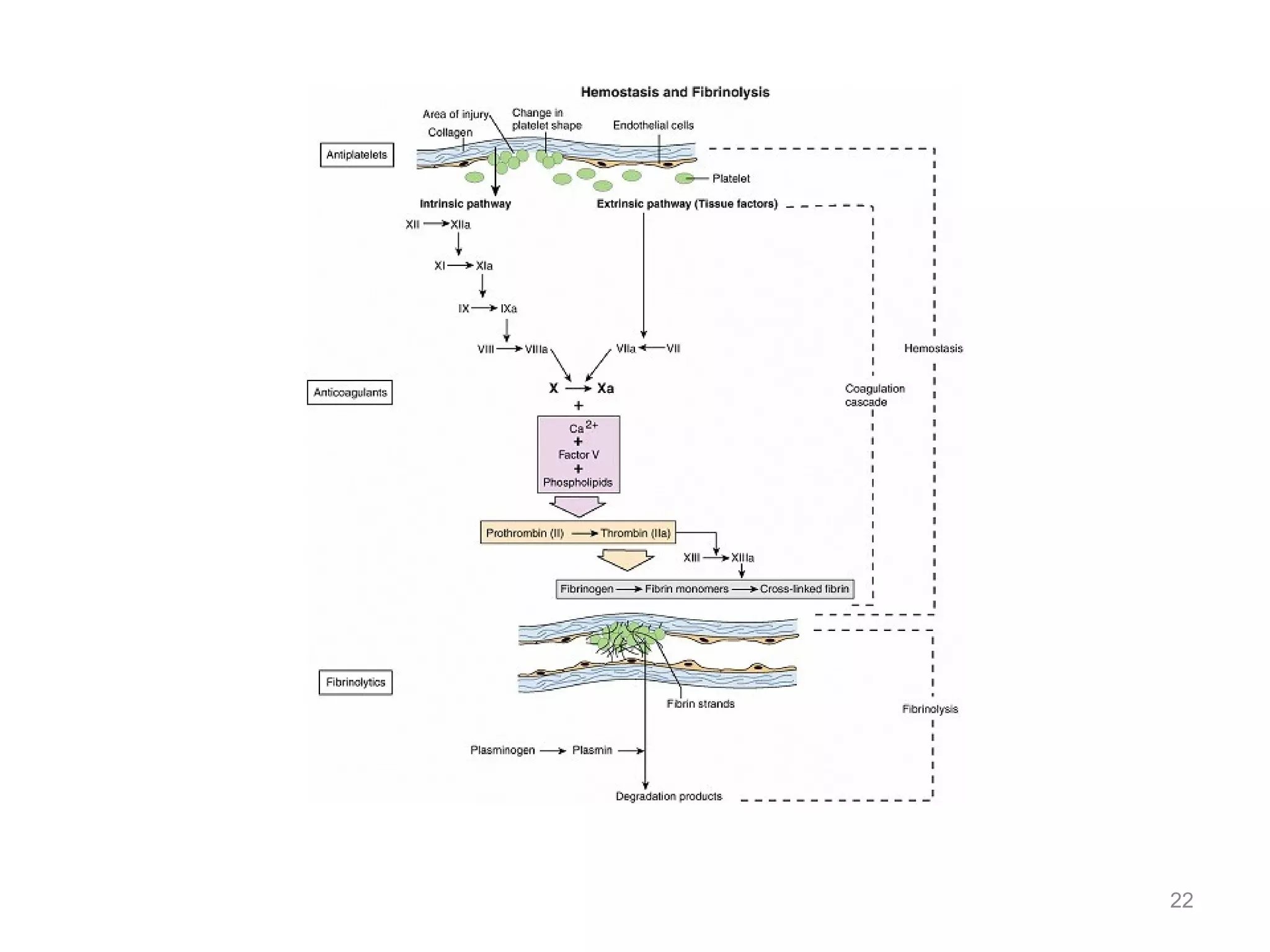
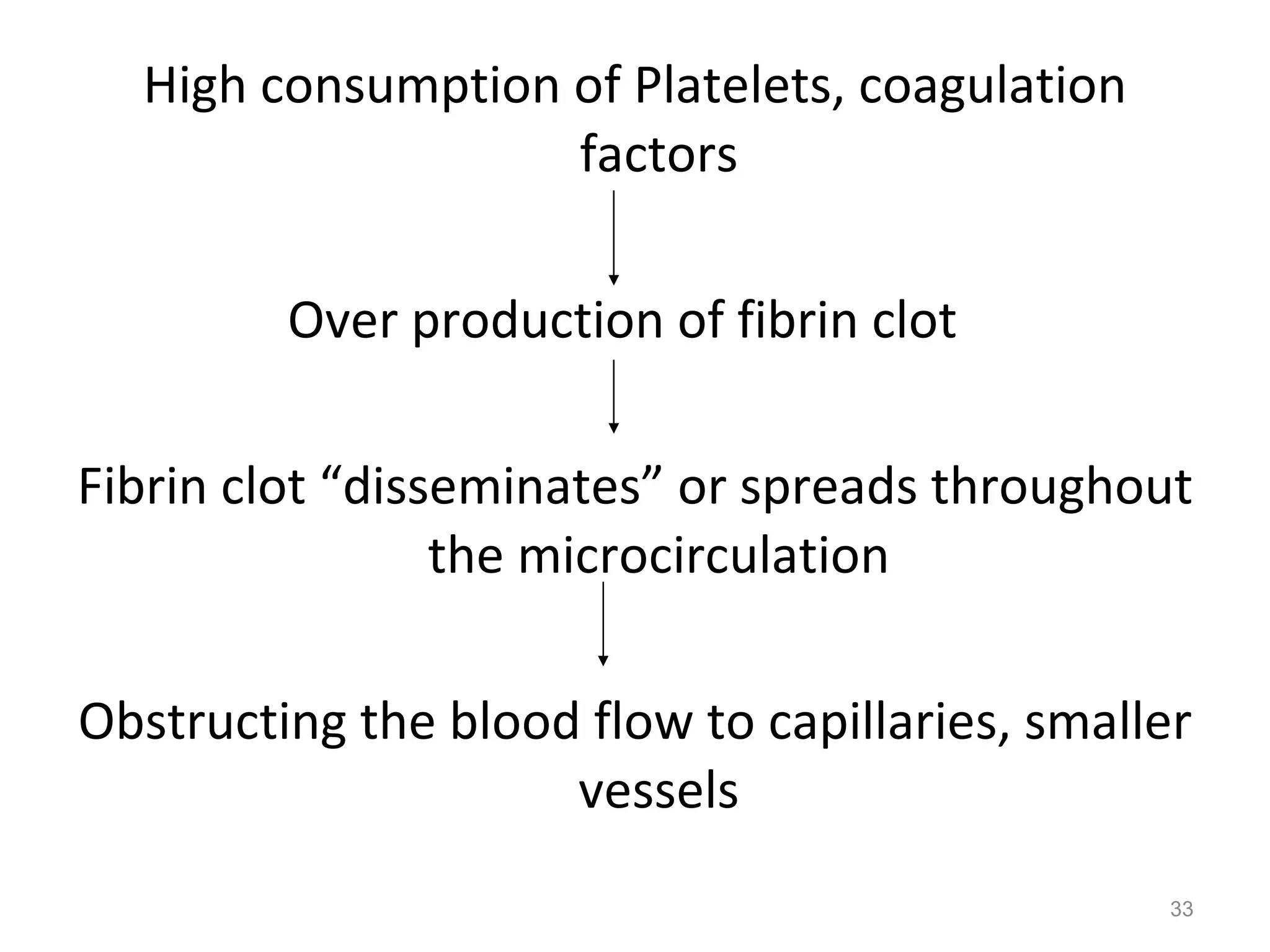
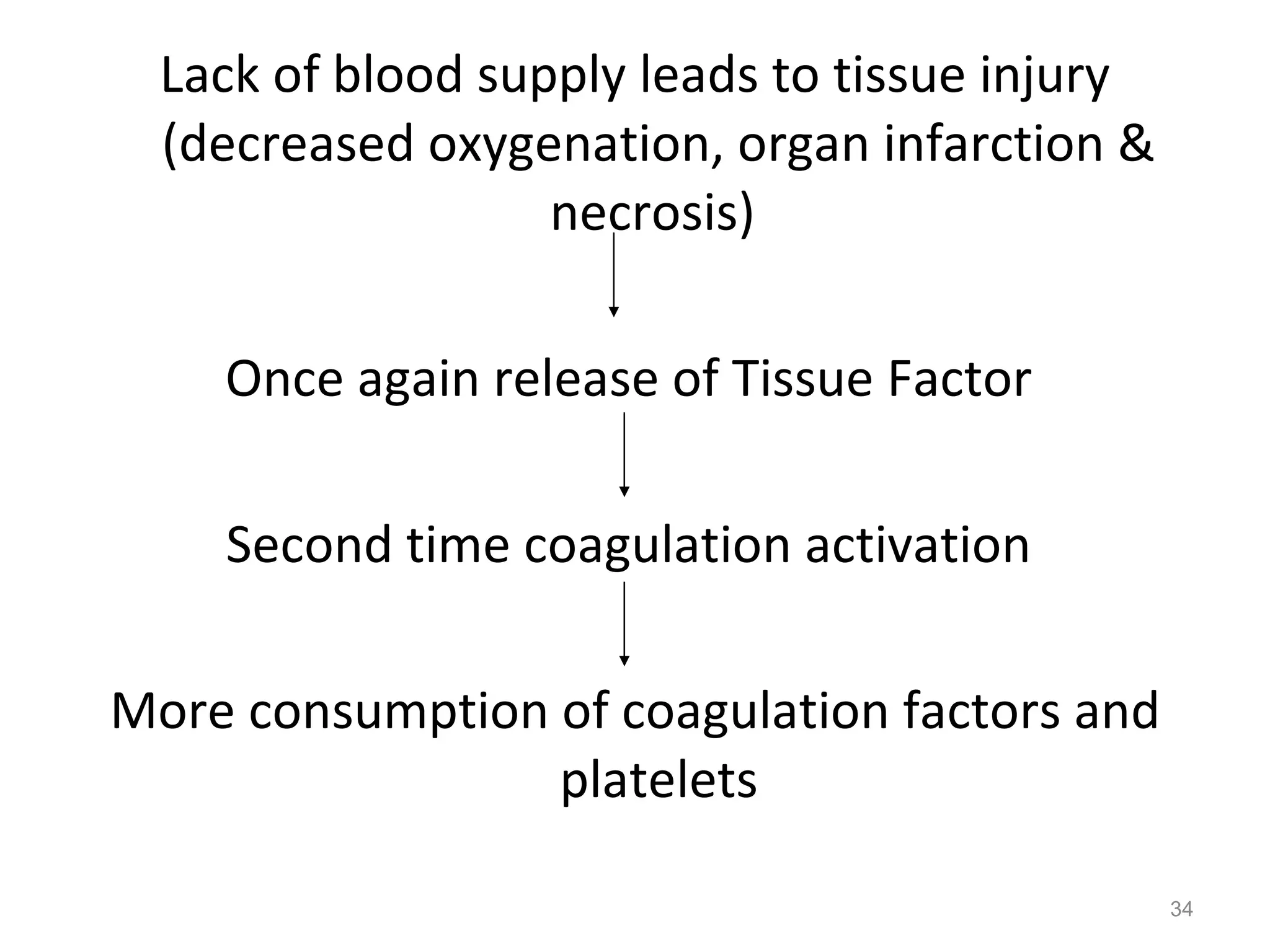
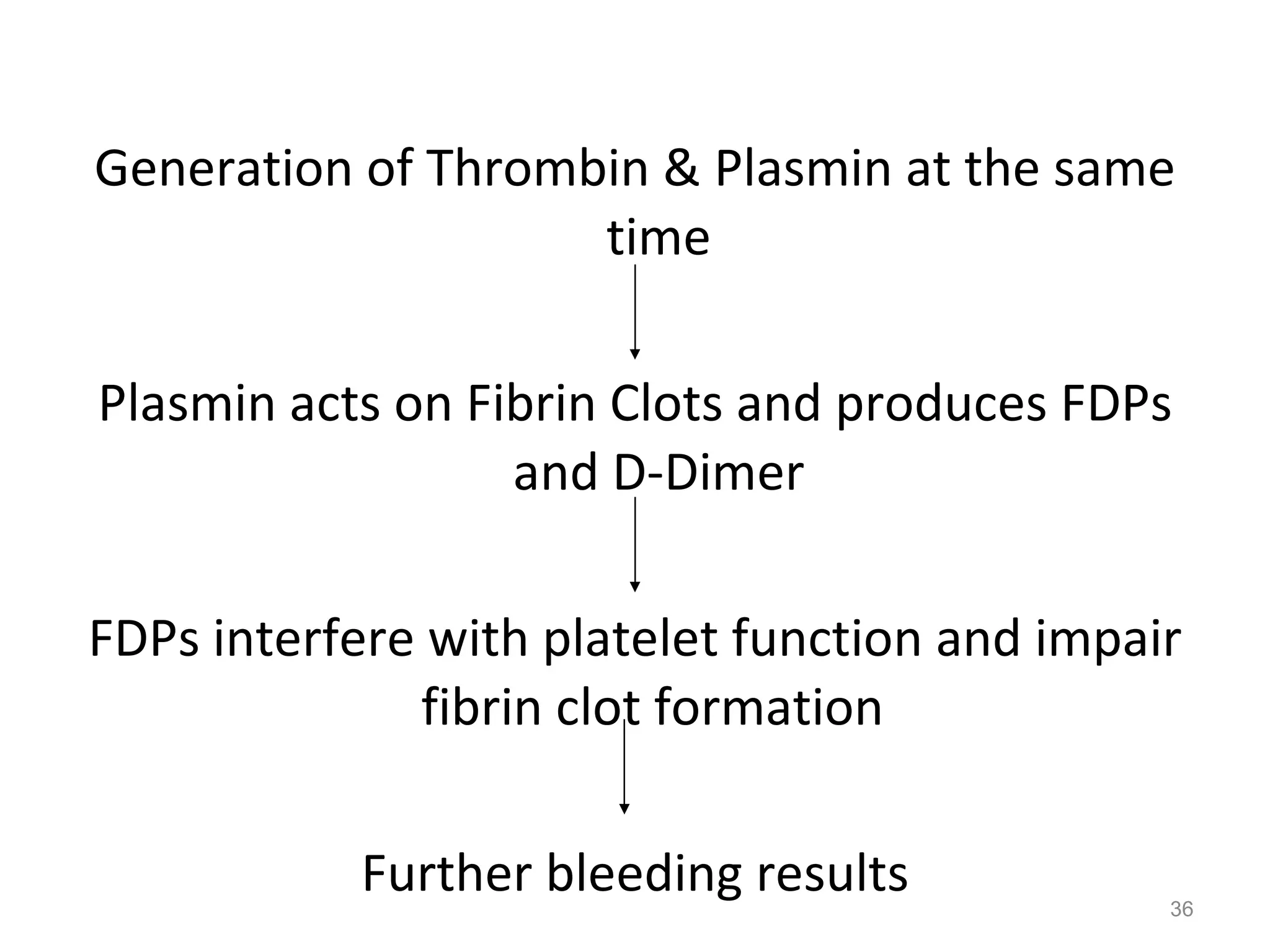
This document summarizes normal hemostasis and abnormalities that can lead to thrombosis or bleeding disorders. It describes the intrinsic and extrinsic coagulation pathways, factors involved, and tests used to evaluate them. Abnormalities in these pathways can cause bleeding disorders like hemophilia or thrombosis. Disseminated intravascular coagulation is also discussed, where initial thrombosis leads to widespread activation of coagulation and bleeding. Treatment options like oral anticoagulants, heparin, and fibrinolytics are mentioned.



















![Thanks Please send your feedbacks to: Priyank Dubey Ph: 09999990845 [email_address] Application Specialist](https://image.slidesharecdn.com/pt-aptt-1218181287688715-8-100323232104-phpapp02/75/Pt-Aptt-1218181287688715-8-42-2048.jpg)