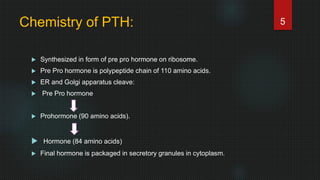
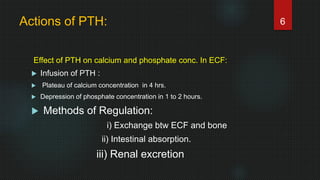
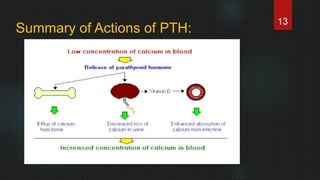
Parathyroid hormone (PTH) is secreted by the parathyroid glands in response to low blood calcium levels. PTH regulates calcium and phosphate concentrations in the body by increasing their absorption in the intestines and kidneys and mobilizing calcium from bones. PTH is synthesized as a precursor protein that is cleaved into the active 84 amino acid hormone. PTH acts to raise blood calcium levels by increasing its resorption from bone, reducing its renal excretion, and enhancing intestinal absorption. Abnormalities in PTH secretion can cause hypo- or hyperparathyroidism, disrupting calcium homeostasis and potentially resulting in symptoms like weakness, pain, and kidney stones.