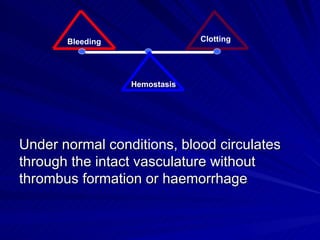
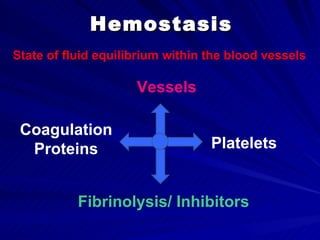
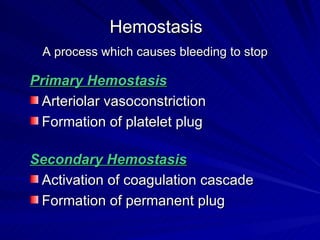
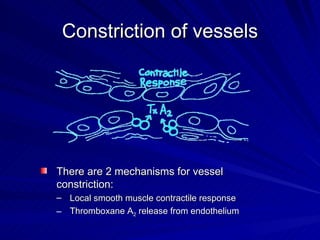
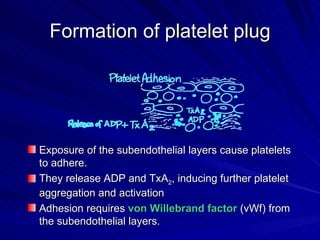
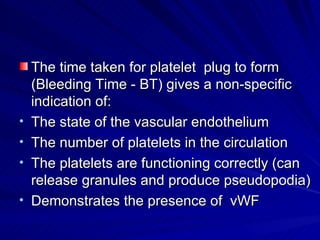
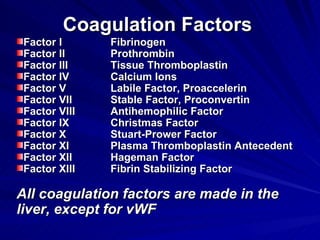
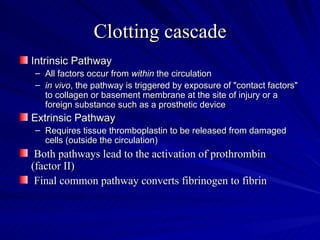
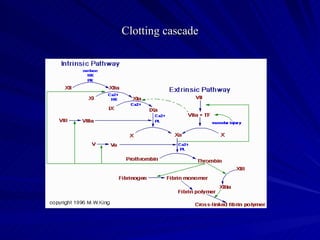
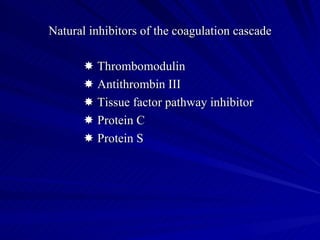
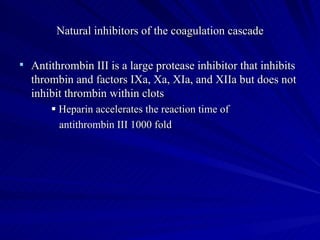
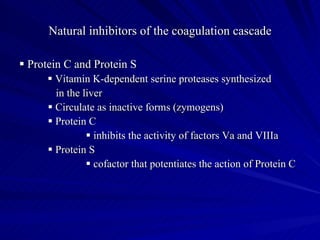
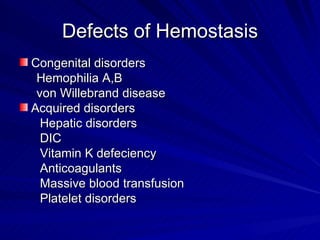
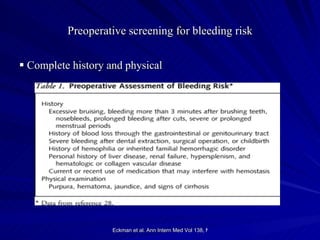
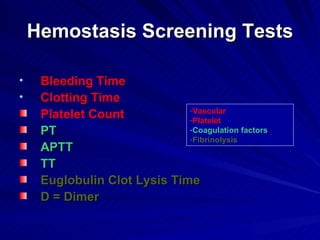
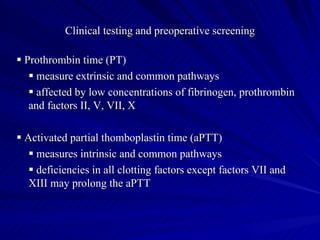
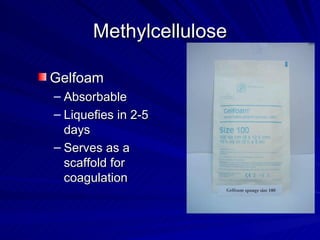
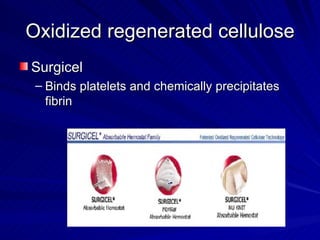
This document discusses hemostasis in surgical patients. It begins by defining hemostasis as the state of fluid equilibrium within blood vessels. It then describes the two mechanisms of hemostasis - primary hemostasis involving vasoconstriction and platelet plug formation, and secondary hemostasis involving activation of the coagulation cascade and formation of a fibrin clot. The document outlines the coagulation cascade and its natural inhibitors. It discusses various defects of hemostasis, preoperative screening tests for bleeding risk, and strategies to achieve surgical hemostasis including direct pressure, cauterization, packing, topical hemostats, and fibrin glue.