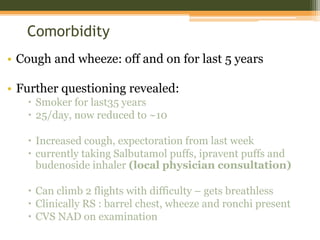
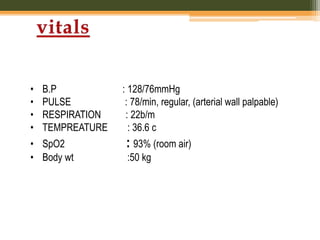
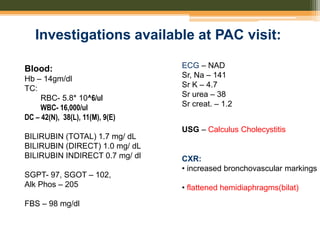
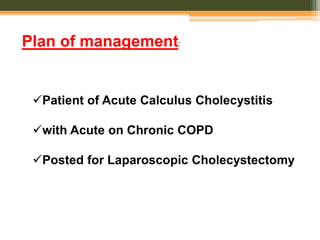
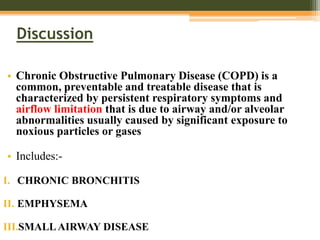
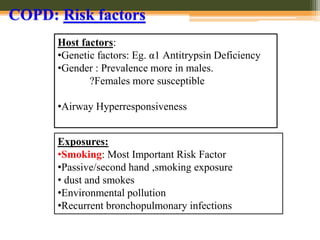
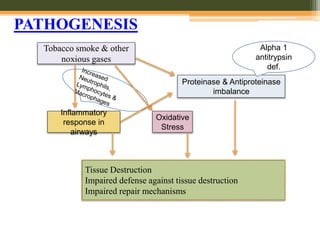
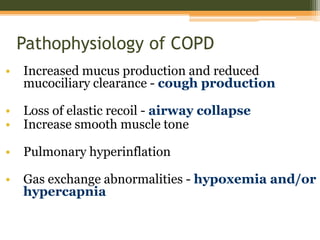
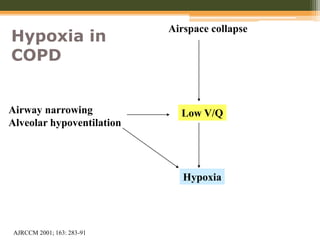
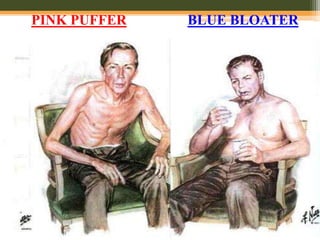
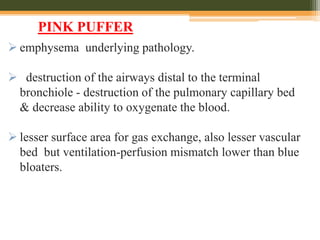
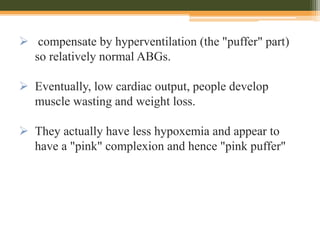
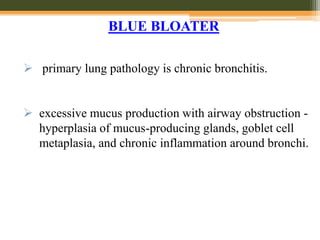
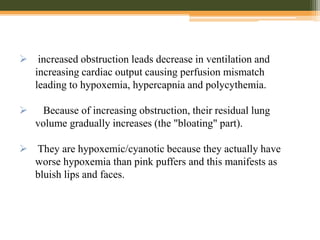
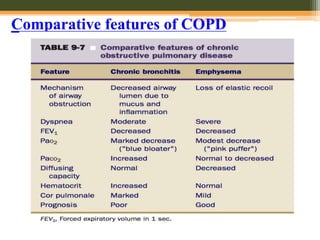
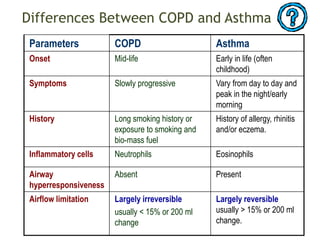
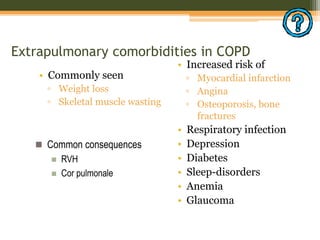
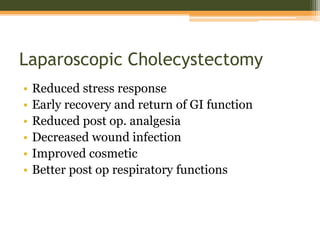
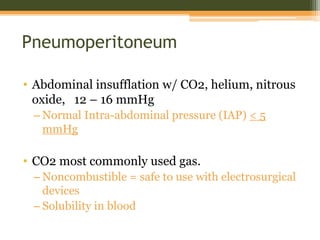
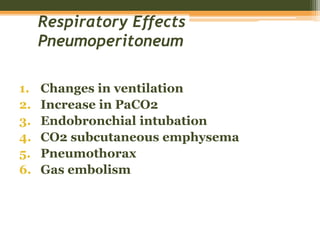
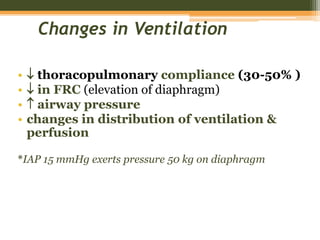
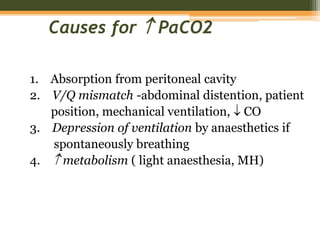
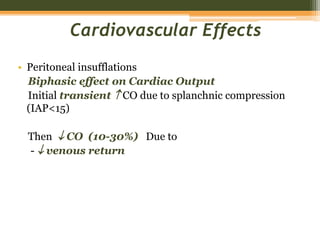
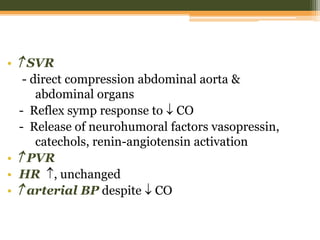
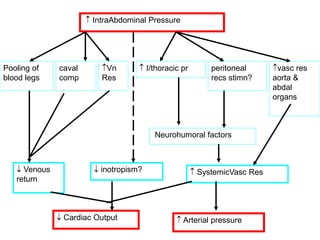
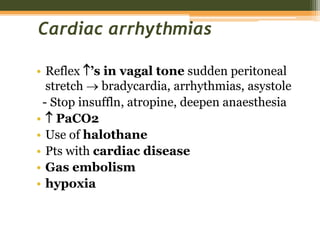
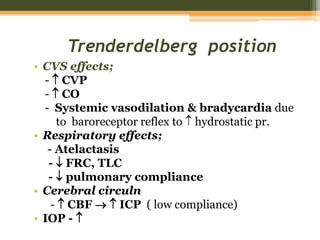
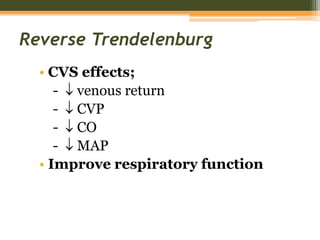
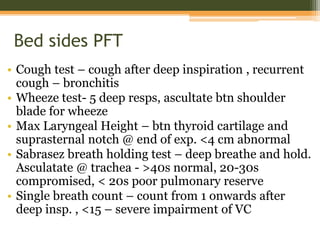
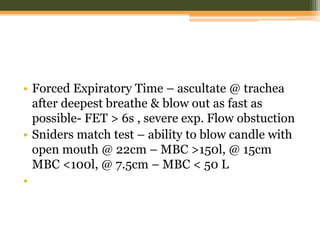
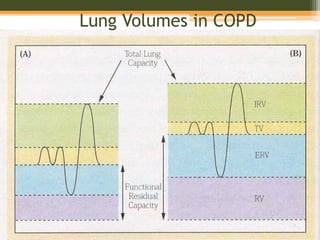
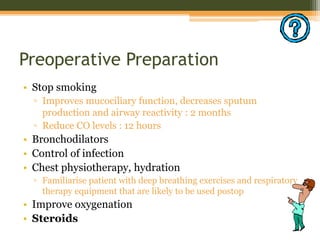
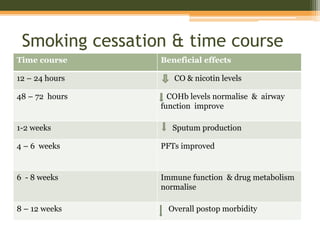
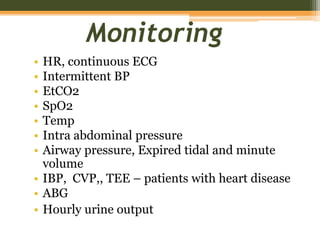
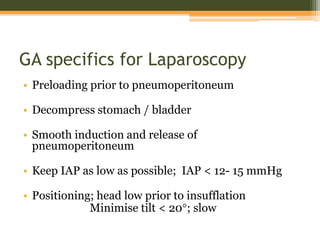
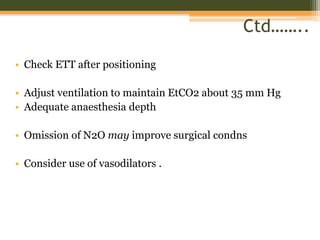
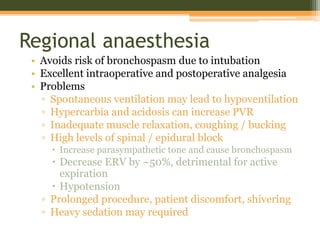
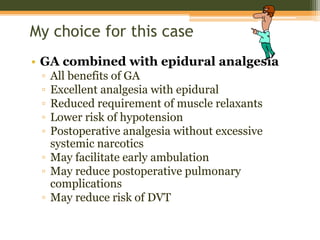
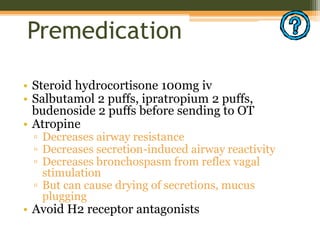
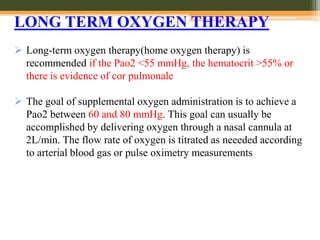
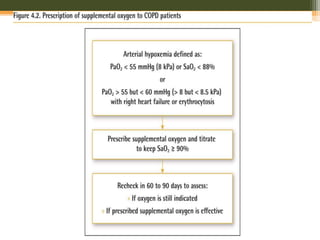
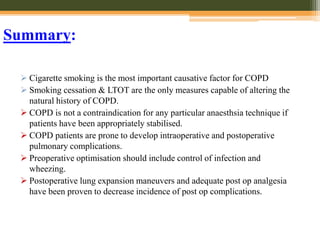
This document discusses anesthetic considerations for laparoscopic cholecystectomy in a patient with COPD. It provides background on the patient's history and comorbidity of COPD. It then summarizes the key respiratory effects of pneumoperitoneum during laparoscopy including increased airway pressures and changes in ventilation. It also discusses the cardiovascular effects, including a transient increase then decrease in cardiac output due to changes in venous return. Finally, it notes other potential risks such as respiratory acidosis, endobronchial intubation, subcutaneous emphysema, and hypothermia that the anesthesiologist must consider in a patient with COPD undergoing laparoscopic surgery.