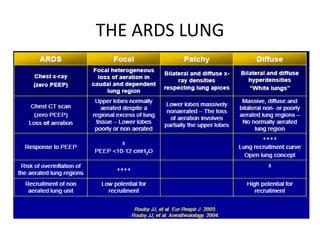
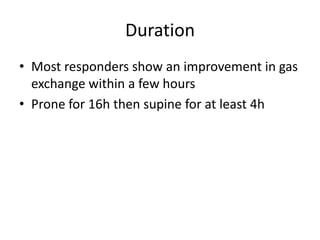
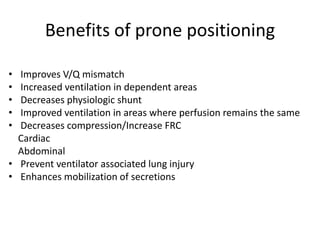
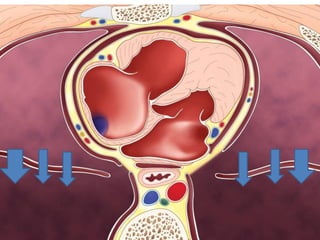
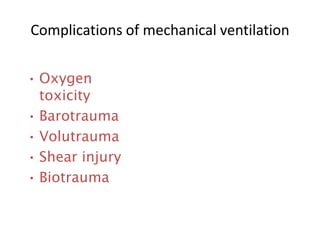
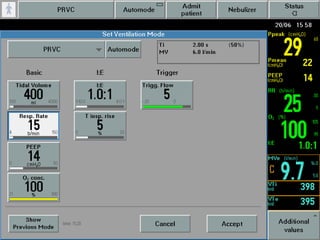
This document discusses strategies for mechanical ventilation in patients with acute respiratory distress syndrome (ARDS). It recommends using a protective ventilation strategy with low tidal volumes between 4-6 ml/kg and limiting airway plateau pressure to below 30 cmH2O to prevent ventilator-induced lung injury. Prone positioning is gaining acceptance as a standard of care for severe ARDS as it improves oxygenation and mortality outcomes. Early application of prone positioning for at least 16 hours per session is recommended for eligible ARDS patients meeting criteria. Recruitment maneuvers combined with high positive end-expiratory pressure are also advocated as part of an "open lung" approach to maximize aeration and oxygenation while minimizing pressures and volumes.
























![Protective Ventilation Strategy in ARDS
• Keep the PaO2 55-80 mmHg
• Maintain an arterial oxygen saturation (SaO2) of 88-94%
• Avoid volutrauma, barotraumas and biotrauma (VIL), by keeping the tidal volumes in the 4-6ml/kg
range and airway plateau pressure < 30 cmH2O .
• Predicted body weight in kg, calculated by: [2.3 *(height in inches - 60) + 45.5 for women or + 50
for men].
* PEEP values of 2cmH2O above PEEP associated with optimal compliance
• Higher respiratory rate.
• PH ≥ 7.15](https://image.slidesharecdn.com/hanaaards-180220163656/85/ARDS-management-29-320.jpg)