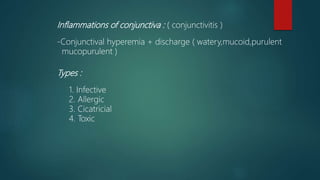
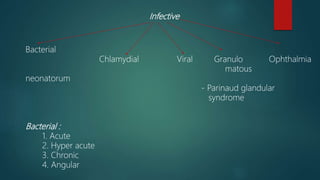
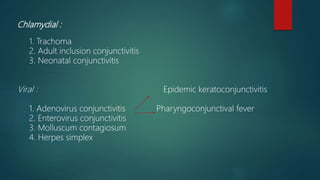
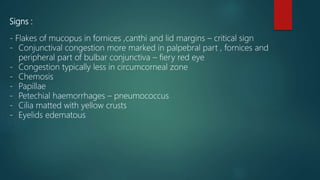
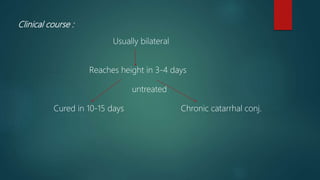
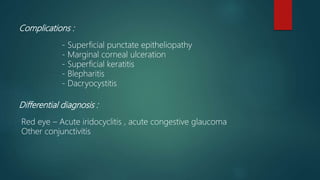
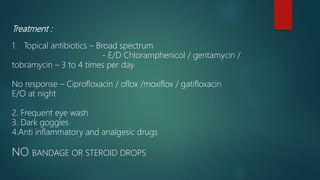
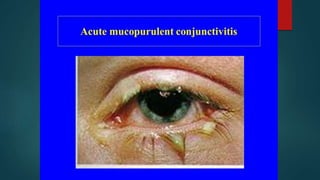
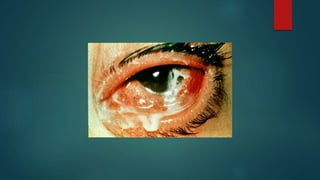
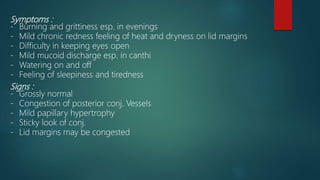
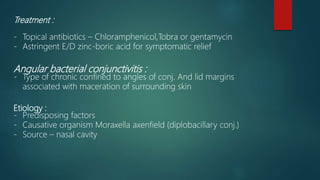
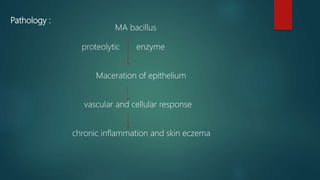
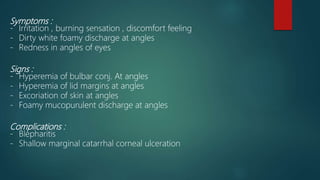
This document discusses various types of conjunctivitis including bacterial conjunctivitis. It describes acute bacterial conjunctivitis as being caused by bacteria like Staphylococcus aureus and presenting with symptoms of discomfort, redness, and mucopurulent discharge. Hyperacute bacterial conjunctivitis includes adult purulent conjunctivitis caused by Neisseria gonorrhoeae presenting with severe pain, swelling, and copious purulent discharge, as well as ophthalmia neonatorum which can be caused by gonorrhea, staphylococcus, or chlamydia in infants. Chronic bacterial conjunctivitis is also discussed as being caused by staphylococcus or gram-negative bacteria