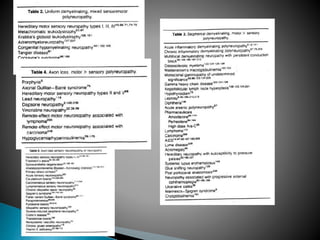
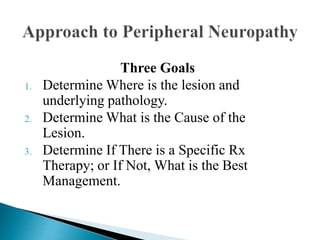
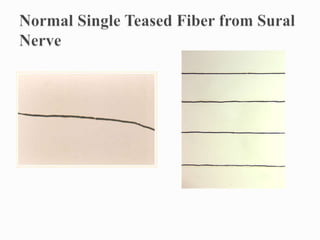
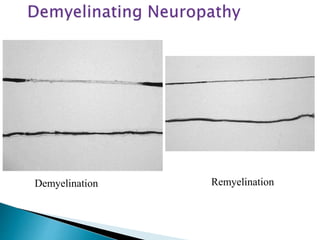
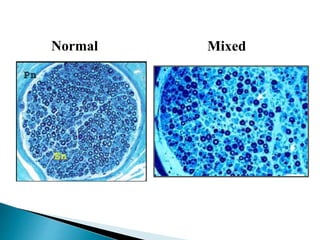
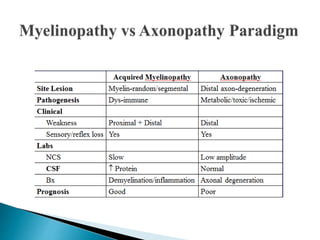
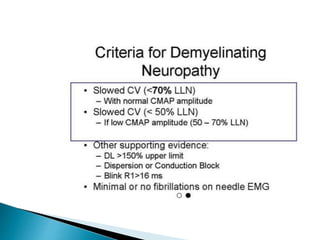
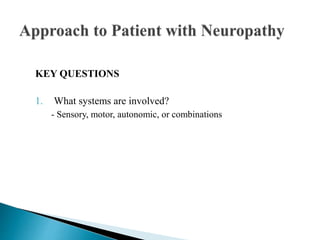
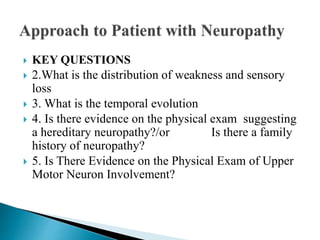
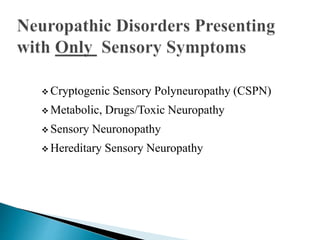
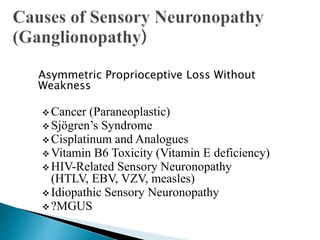
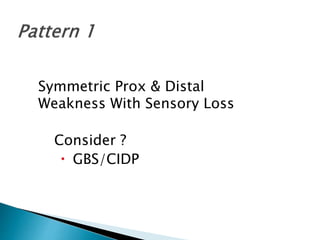
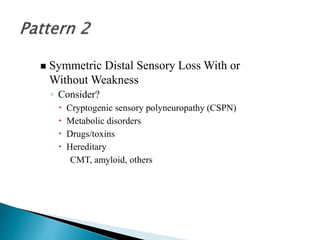
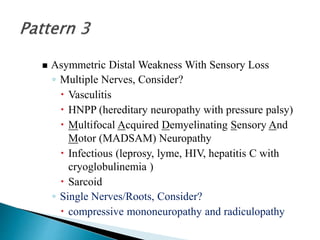
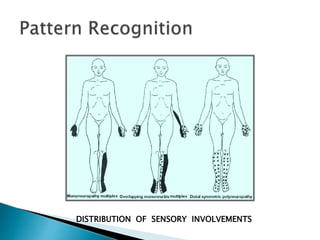
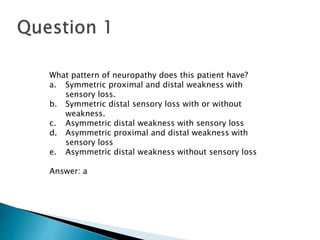
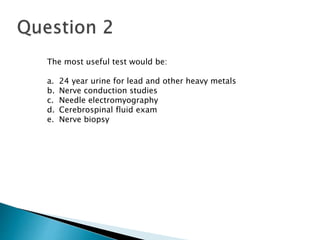
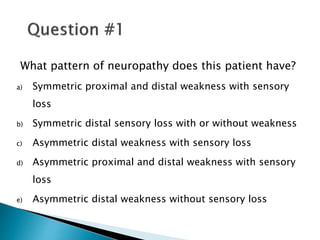
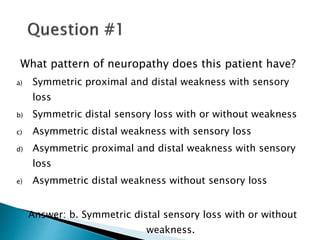
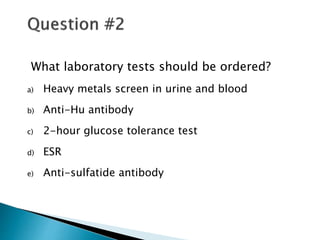
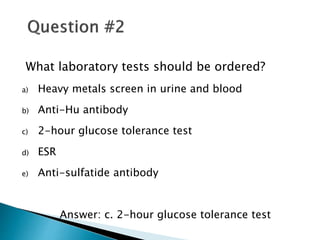
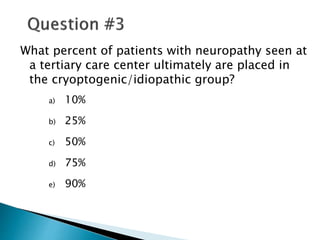
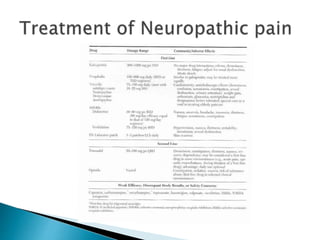
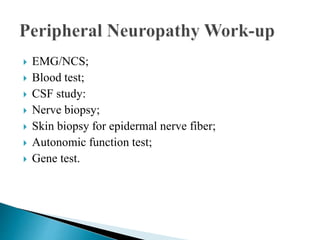
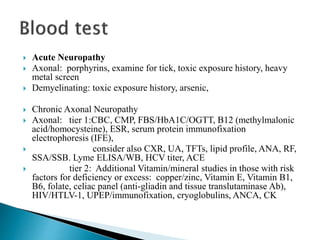
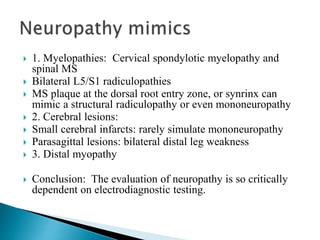
The document outlines an approach to peripheral neuropathy by discussing three main goals: determining the lesion location and pathology, identifying the cause of the lesion, and determining if there is a specific treatment or best management approach. It then reviews different patterns of neuropathies including myelinopathies, axonopathies, demyelination, remyelination, and discusses key questions to consider in the evaluation of peripheral neuropathies.