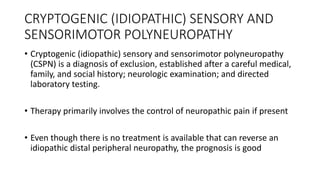
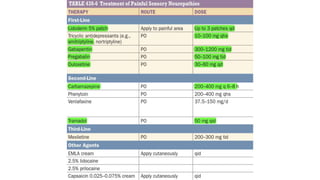
Peripheral neuropathies can affect the cell body, myelin sheath, or axon. When evaluating a patient with neuropathy, the clinician aims to identify where the lesion is located, determine the cause, and prescribe proper treatment. Electrodiagnostic studies and nerve biopsies help classify the neuropathy and diagnose underlying causes like diabetes, autoimmune diseases, toxins, vitamins deficiencies, infections, and malignancies. Cryptogenic neuropathies have no known cause and treatment focuses on managing neuropathic pain symptoms.