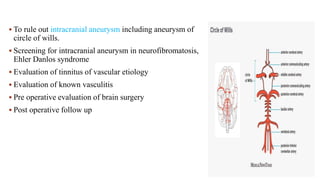
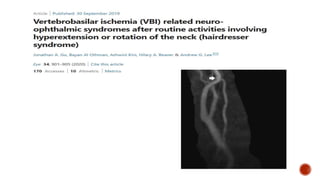
This document provides an overview of magnetic resonance angiography (MRA). It discusses the physics behind MRA, different techniques used including time-of-flight imaging and phase contrast imaging, as well as considerations for patient preparation and contraindications. Advantages of MRA include being non-invasive and avoiding risks associated with conventional angiography such as damage to arteries. Limitations include inability to depict small vessels or slow blood flow as well as conventional methods. Overall, the document provides a comprehensive introduction to MRA.









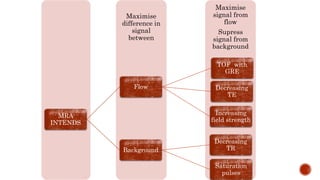










![TOF MRA is based on the differences in saturation between the extravascular
and intravascular (moving blood) constituents.
A gradient pulse is repeatedly applied to a slice/slab (two-dimensional
[2D]/three-dimensional [3D]) of tissue.
The signal intensity of static tissue (extravascular) is progressively suppressed
by repetitive radio frequency pulses, the signal from the stationary tissue
decreases and becomes more saturated with each pulse.
The moving blood brings unsaturated protons into the tissue slice, which
generates a high signal intensity. and the inflow enhancement in the investigated
vessel produces the angiographic effect.](https://image.slidesharecdn.com/mramrv-210809135340/85/Mra-mrv-21-320.jpg)