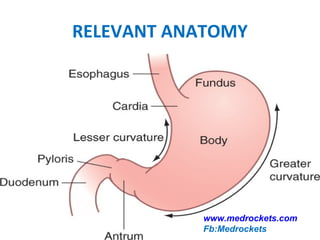
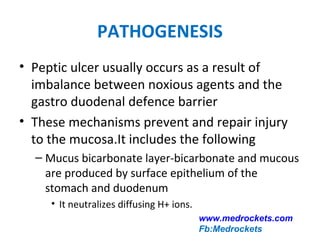
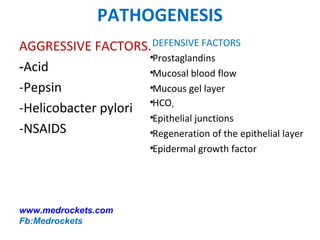
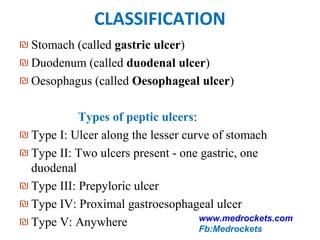
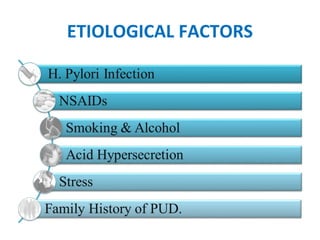
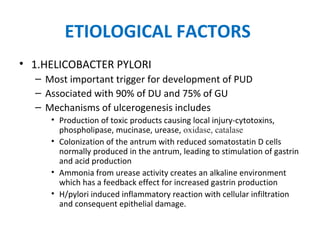
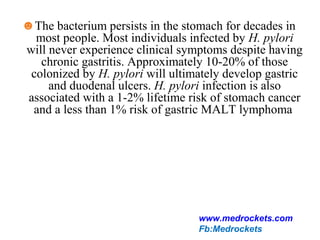
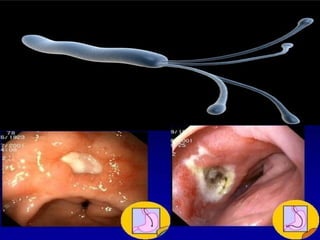
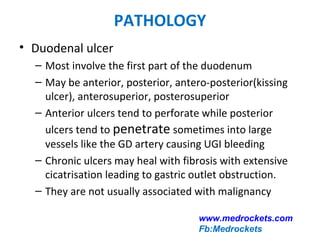
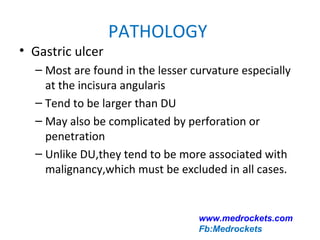
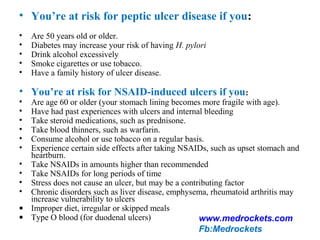
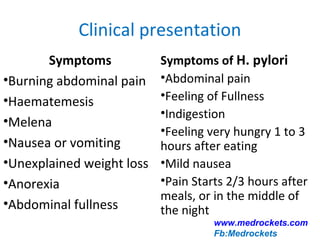
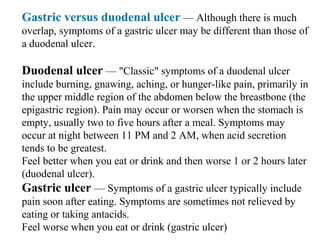
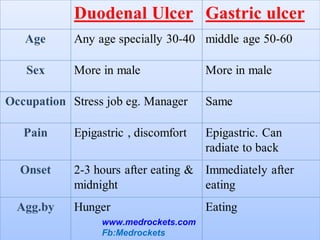
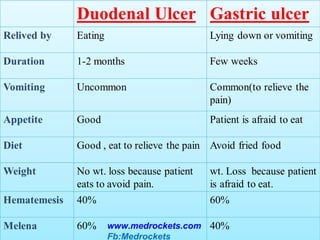
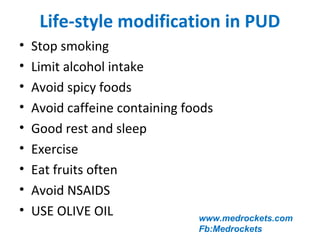
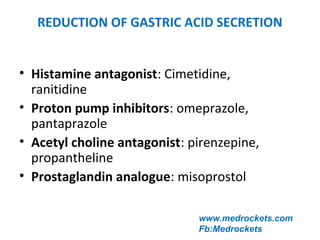
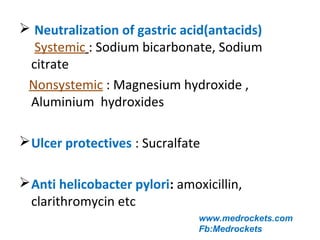
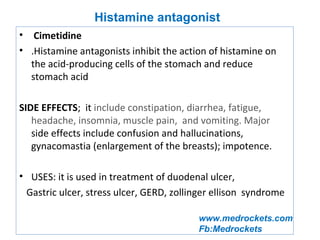
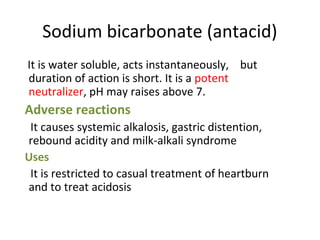
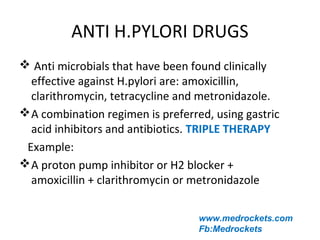
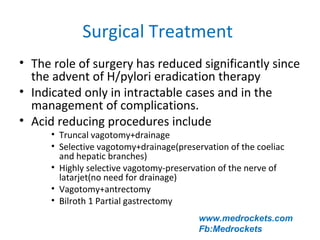
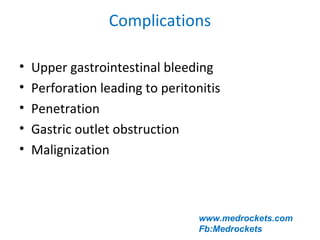
Peptic ulcer disease is caused by an imbalance between damaging factors like gastric acid and protective mucosal defenses. It manifests as ulcers in the stomach or duodenum. Key causes include Helicobacter pylori infection in over 80% of cases, and NSAID use. Symptoms vary depending on the ulcer location but commonly include abdominal pain relieved by food or antacids. Diagnosis involves endoscopy while treatment focuses on eradicating H. pylori, reducing acid with PPIs, lifestyle changes, and symptom relief.