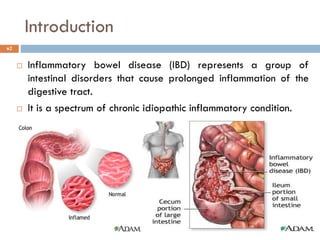
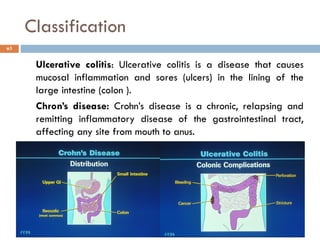
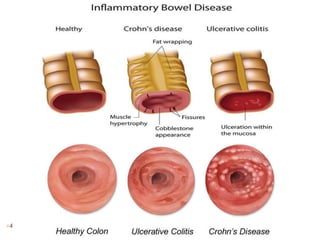
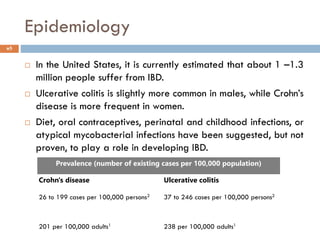
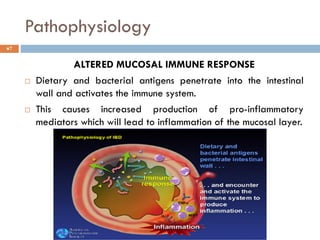
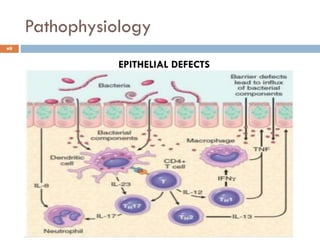
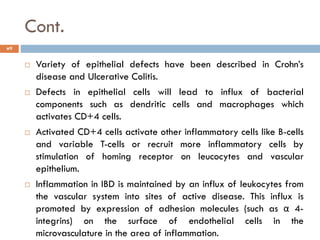
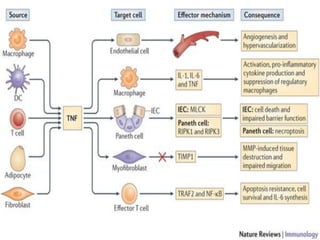
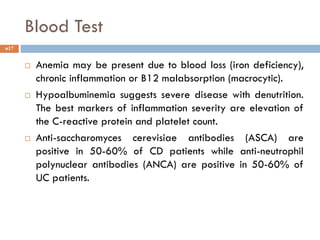
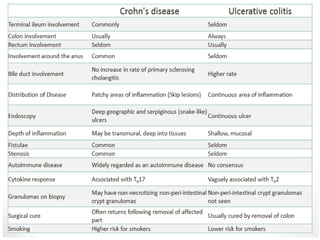
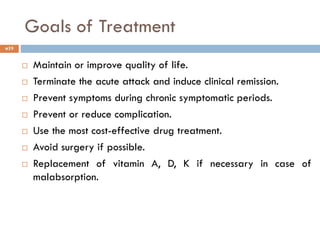
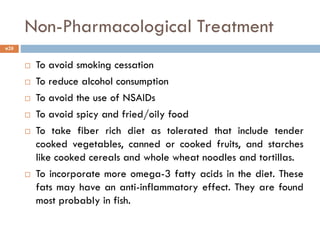
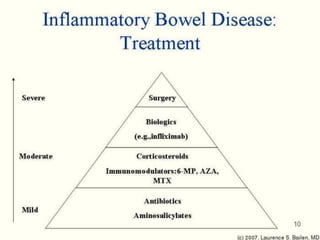
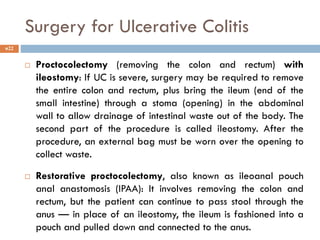
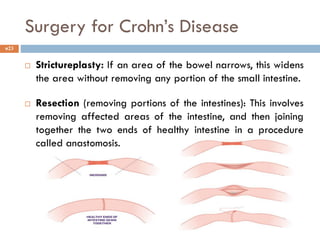
The document provides information on inflammatory bowel disease (IBD), including its classification into ulcerative colitis and Crohn's disease. It discusses the epidemiology, etiology, pathophysiology, clinical manifestations, diagnosis, treatment goals, and pharmacological and non-pharmacological treatment approaches for IBD. The major drug therapy types used for IBD include aminosalicylates, corticosteroids, immunosuppressants, TNF inhibitors, and antimicrobials. Surgery may be required for severe cases or complications that do not respond to medical management.