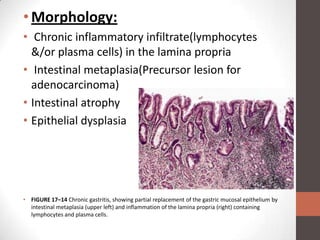
This document summarizes acute and chronic gastritis. Acute gastritis is caused by factors like NSAID use, alcohol, smoking, infections, and stress. It involves neutrophil infiltration and can cause erosions and ulceration. Chronic gastritis is defined by long-term inflammation leading to atrophy and intestinal metaplasia. Helicobacter pylori infection is a major cause and results in urease production and cytotoxins that drive chronic inflammation. Autoimmune mechanisms can also lead to chronic gastritis, seen as lymphocytes and plasma cells in the lamina propria and intestinal metaplasia.