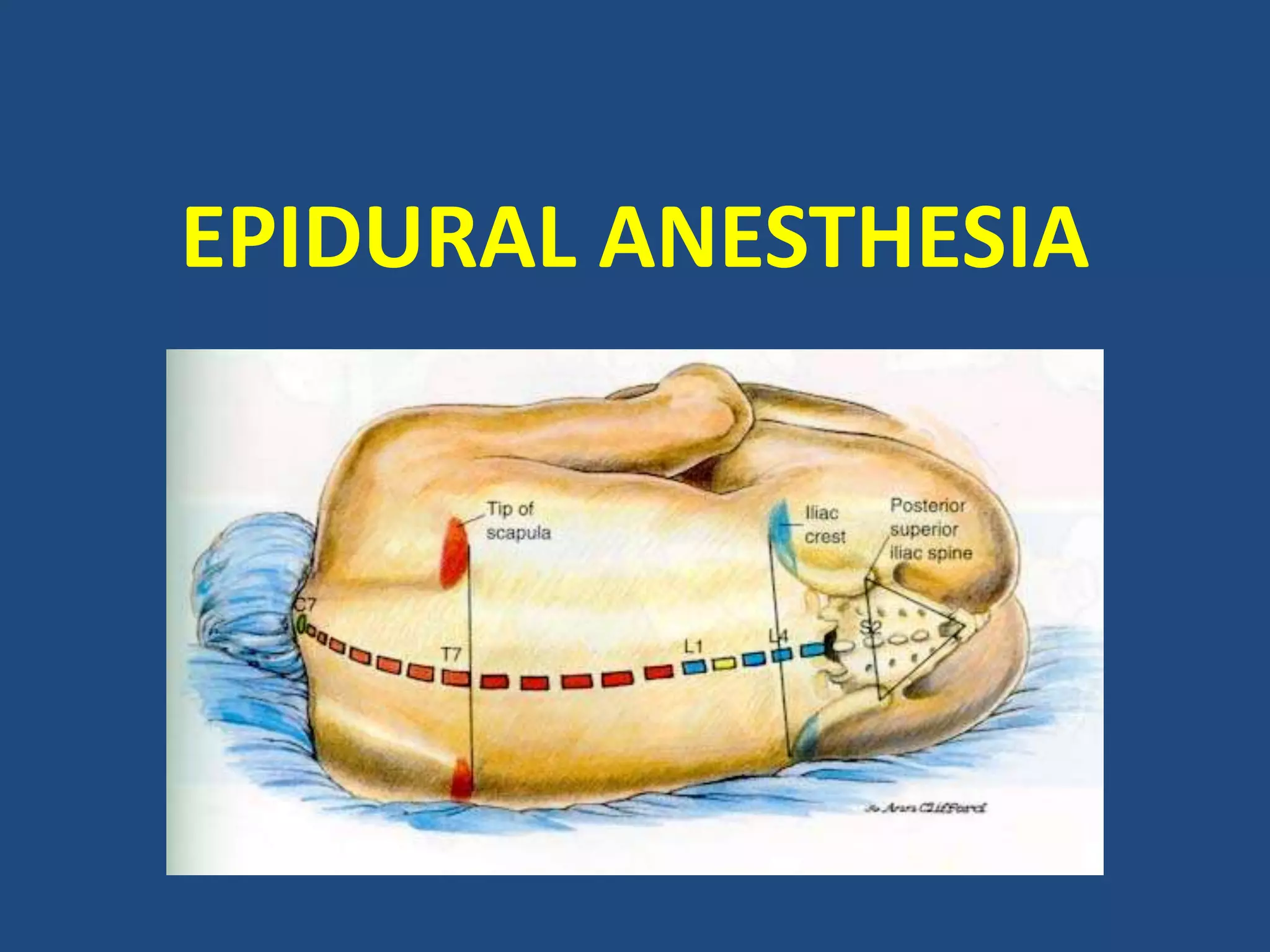
Epidural anesthesia blocks pain in a specific region of the body by administering local anesthetics into the epidural space surrounding the spinal cord. This results in decreased sensation in the lower half of the body. Epidural anesthesia can be performed at different spinal levels and provides pain relief rather than total lack of sensation. It allows for selective nerve blockade and is commonly used for operations below the diaphragm when general anesthesia is contraindicated or for post-operative pain relief.