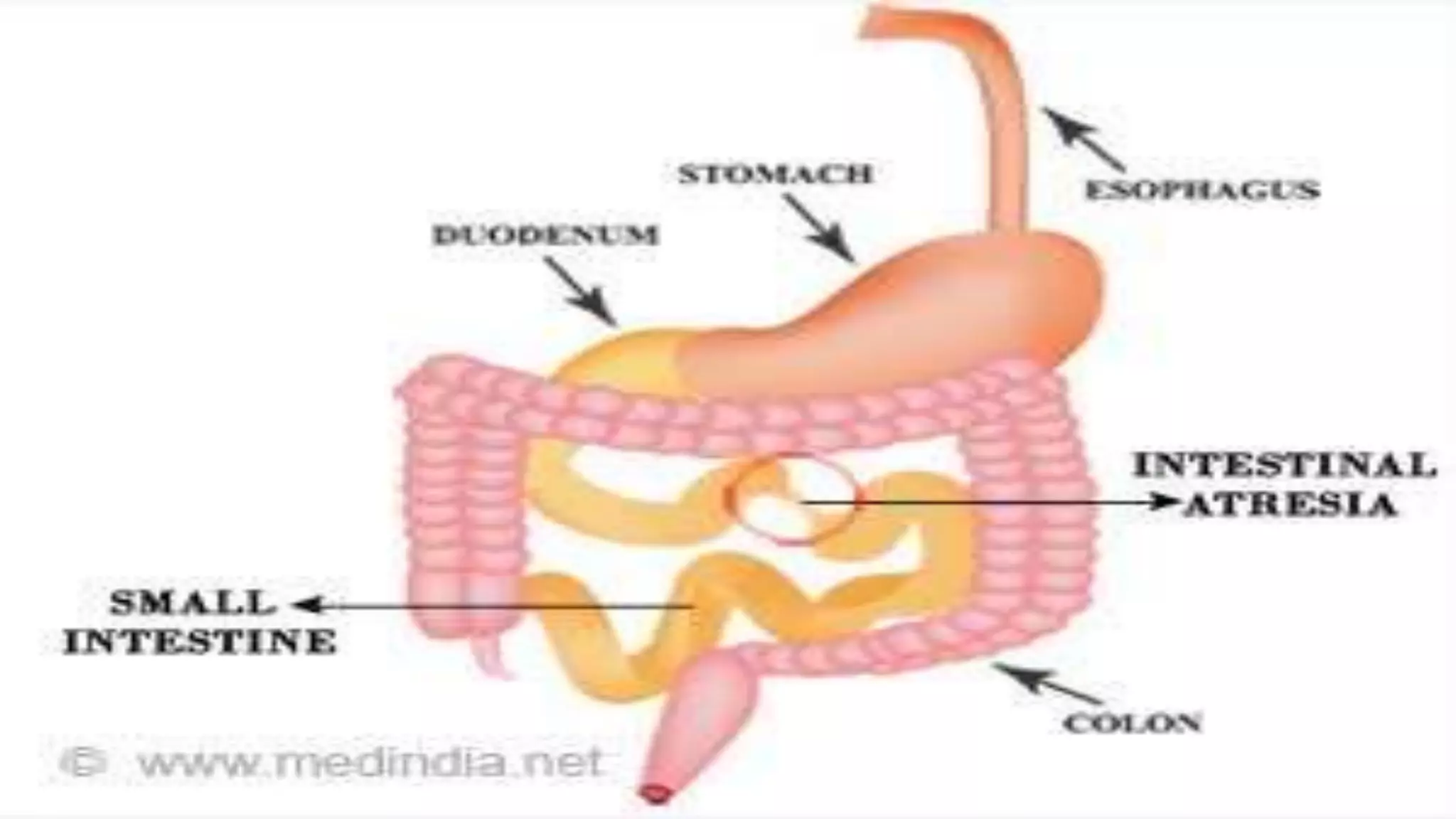
Intestinal obstruction occurs when the intestine is blocked, preventing normal movement of its contents. It can be caused by mechanical blockages such as tumors or hernias, or functional issues like neuromuscular problems. Symptoms include abdominal pain, vomiting, distension and constipation. Treatment involves fluid resuscitation, antibiotics, pain management, and sometimes surgery to remove the obstruction. Proper diagnosis and timely treatment are important to prevent complications like perforation and sepsis.