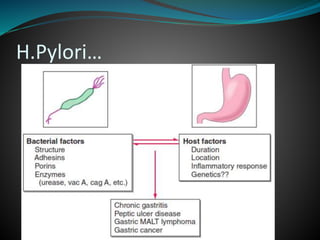
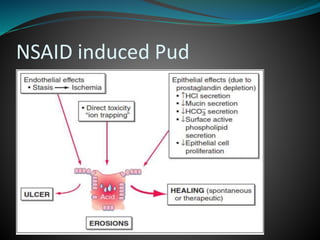
This document outlines a lecture on peptic ulcer disease (PUD). It begins with definitions of PUD and ulcers, noting the typical burning pain exacerbated by fasting and relieved by eating. It then discusses gastric physiology including the mucosal defense system and role of prostaglandins. Key causes of ulcers are described as H. pylori bacteria and NSAID use. Clinical features, complications, differential diagnosis, diagnostic tests, and treatment approaches are summarized. The role of H. pylori and NSAIDs in duodenal and gastric ulcers is emphasized throughout.