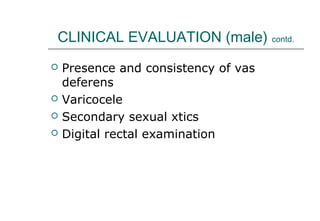
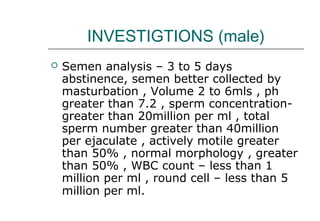
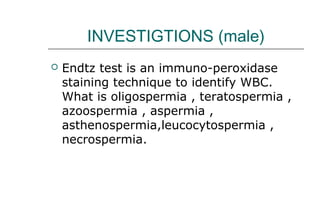
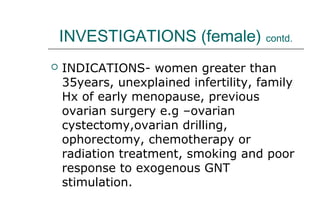
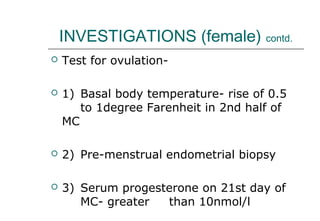
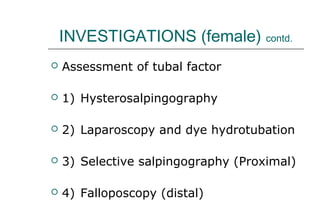
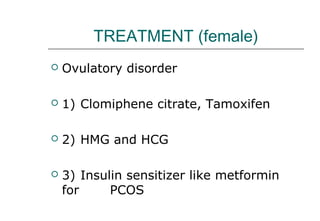
The document discusses infertility, defining it as 1 year of unprotected intercourse without pregnancy. It describes how infertility is classified and evaluated in both males and females. Common causes of infertility are then outlined for both sexes, including factors related to ovulation, the fallopian tubes, uterus, and immune or idiopathic issues. The prevalence of different causes is provided. Clinical evaluation steps and potential investigations for males and females are also summarized. Finally, treatment options are reviewed for resolving infertility in males and females.