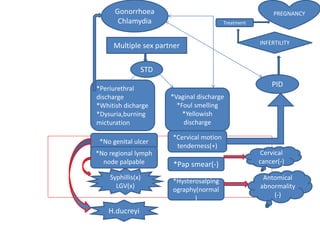
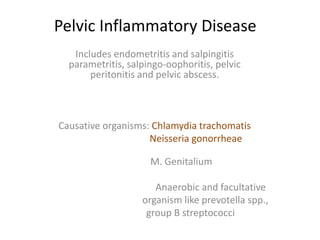
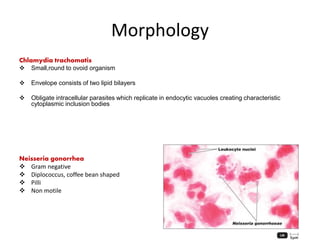
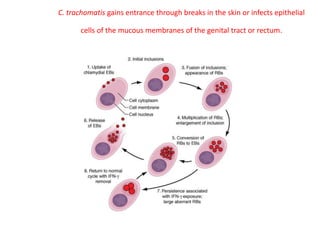
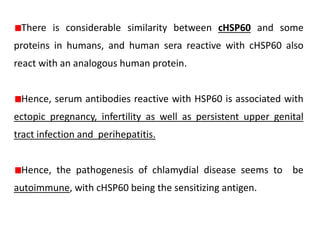
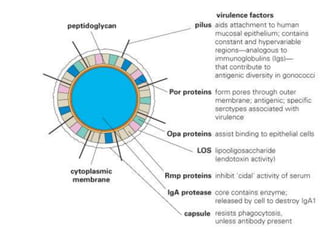
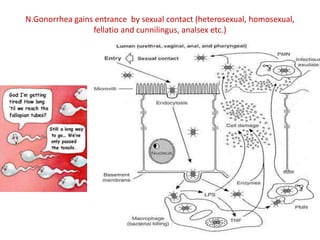
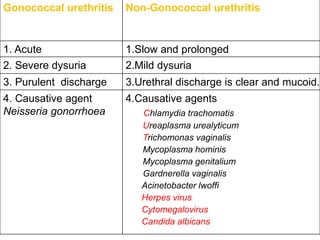
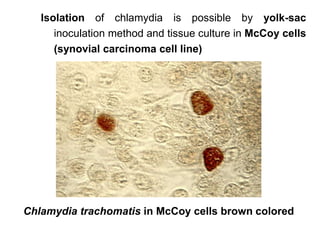
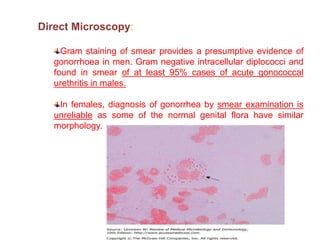
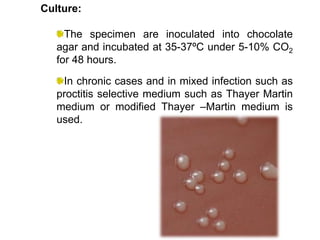
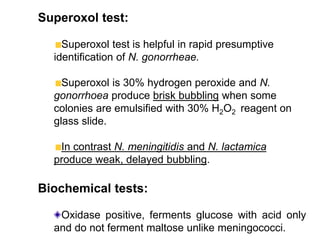
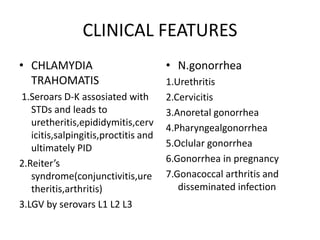
PID is caused by bacteria like Chlamydia trachomatis and Neisseria gonorrheae. C. trachomatis gains entry through breaks in the skin or mucous membranes and causes diseases like urethritis, cervicitis, salpingitis, and PID through an autoimmune response to the cHSP60 antigen. N. gonorrheae enters through sexual contact and causes acute urethritis in males seen as purulent discharge, while in females diagnosis is difficult as normal flora can appear similar. Laboratory diagnosis involves direct detection of antigens, culture, and serology of samples from the urogenital tract.