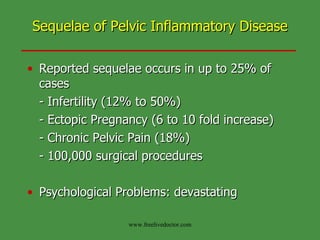
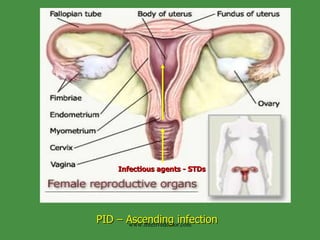
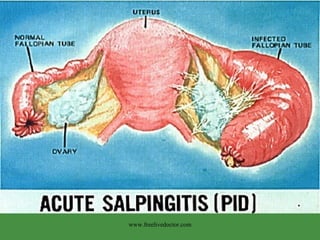
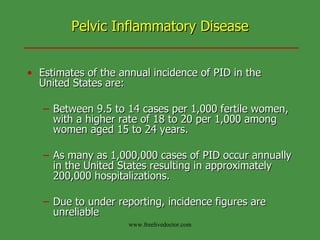
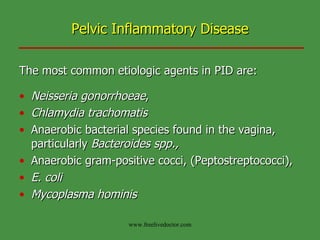
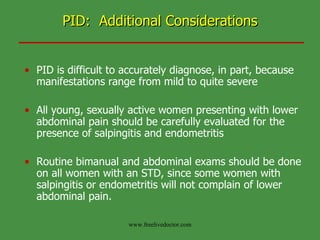
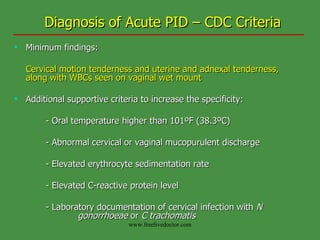
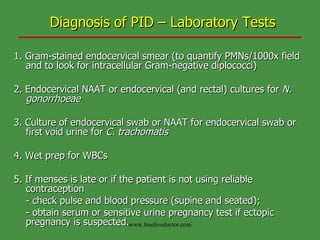
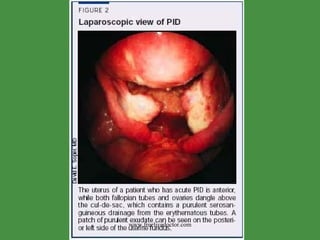
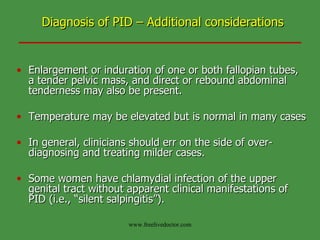
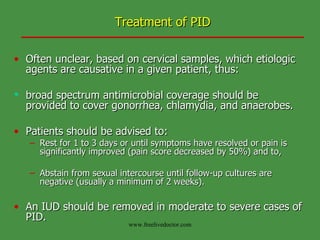
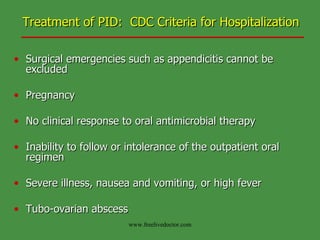
Pelvic inflammatory disease (PID) is an infection of the female upper genital tract that can cause long-term complications like infertility and ectopic pregnancy. Common causes are sexually transmitted bacteria like Chlamydia and gonorrhea. Diagnosis involves examining for cervical tenderness and confirming with tests like endometrial biopsy or laparoscopy. Treatment aims to eliminate the infections with antibiotics and prevent complications through follow up testing and partner treatment. Long term risks counseling is important due to potential issues like chronic pelvic pain.
![CREOG Educational Objectives: Pelvic Inflammatory Disease Treatment of PID with appropriate antimicrobial and surgical options Summarize the potential long-term effects [of PID] and counsel patients regarding the risks of further complications, including: Chronic pelvic pain Infertility Ectopic pregnancy www.freelivedoctor.com](https://image.slidesharecdn.com/pelvicinflammatorydisease-100515014930-phpapp01/85/Pelvic-inflammatory-disease-4-320.jpg)

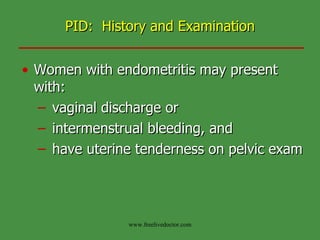
![PID: History and Examination Symptoms suggestive of PID include: Abdominal pain (usually bilateral and in the lower quadrants), Dyspareunia, [abnormal] Vaginal discharge, Menometrorrhagia, Dysuria, Onset of pain in association with menses, Fever, and/or chills Nausea or vomiting www.freelivedoctor.com](https://image.slidesharecdn.com/pelvicinflammatorydisease-100515014930-phpapp01/85/Pelvic-inflammatory-disease-12-320.jpg)

![Outpatient Treatment of PID: CDC Treatment Guidelines 2002 Regimen A Either of the following: - Ofloxacin 400 mg orally twice a day for 14 days - Levofloxacin 500 mg orally once daily, with or without Metronidazole 500 mg orally twice a day for 14 days. Regimen B Any of the following: - Ceftriaxone 250 mg IM once, - Cefoxitin or Cefotetan 2 g IM plus Probenecid, 1 g orally in a single dose, [Other parenteral third-generation cephalosporins (e.g., ceftizoxime or cefotaxime),] plus - Doxycycline 100 mg orally twice a day for 14 days, with or without Metronidazole 500 mg orally twice a day for 14 days. www.freelivedoctor.com](https://image.slidesharecdn.com/pelvicinflammatorydisease-100515014930-phpapp01/85/Pelvic-inflammatory-disease-28-320.jpg)