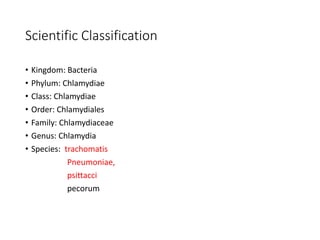
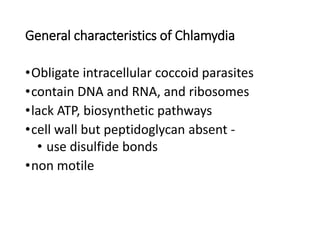
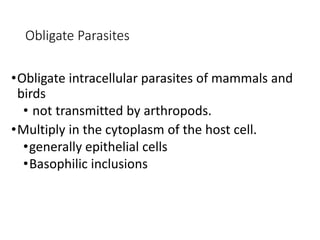
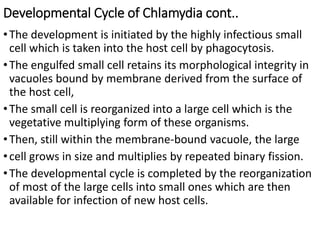
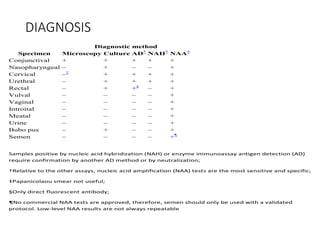
Chlamydia is an obligate intracellular parasite that infects humans and animals. It has two forms - the infectious elementary body and the replicative reticulate body. It causes diseases like trachoma, pneumonia, and lymphogranuloma venereum. Diagnosis involves cell culture, antigen detection, or nucleic acid amplification tests of specimens from infected sites. Treatment is usually with tetracyclines or macrolides. Control relies on treatment of infected individuals and their partners as well as hygiene and quarantine measures.