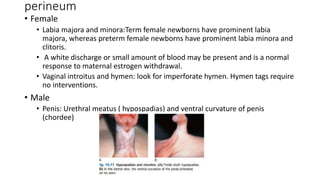
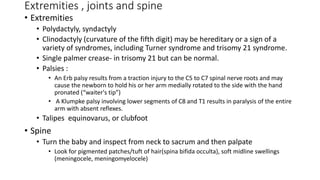
This document provides guidance on performing a newborn examination. It discusses examining the baby's history, vital signs, appearance, major body systems and reflexes. The examination is conducted in a warm, well-lit room and includes assessing temperature, heart rate, respiratory rate, blood pressure, color, muscle tone, reflexes, measurements and a full physical exam from head to toe. The exam evaluates the skin, fontanelles, eyes, ears, heart, lungs, abdomen, genitals, limbs and neurological function through assessing tone and primitive reflexes. The goal is to identify any abnormalities and ensure healthy development.