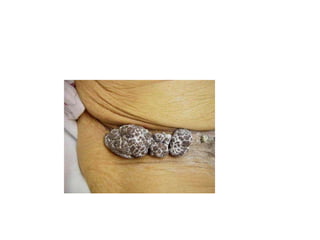
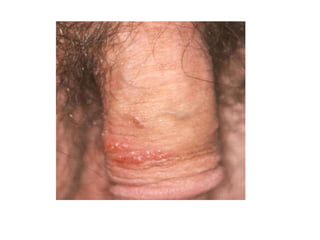
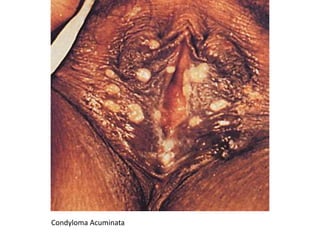
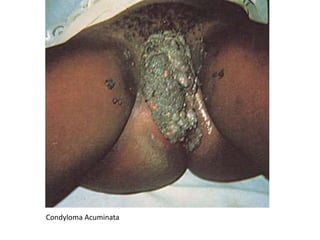
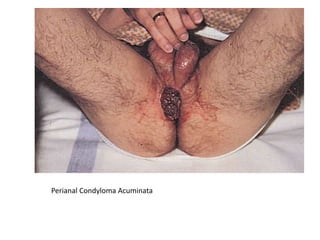
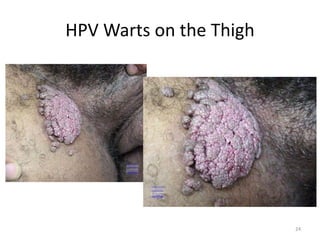
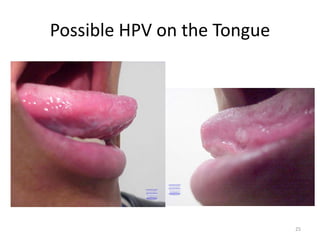
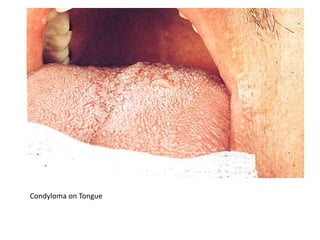
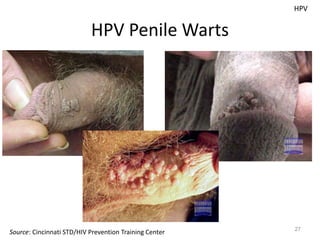
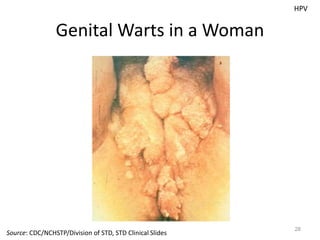
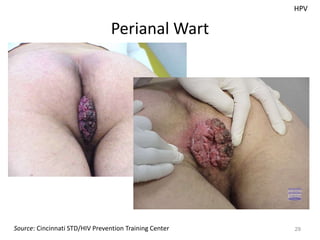
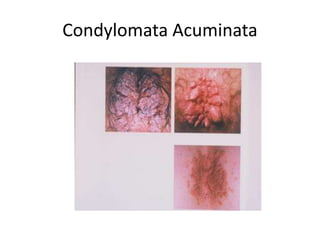
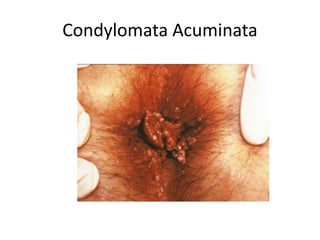
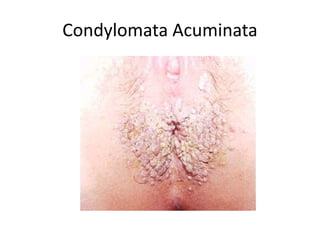
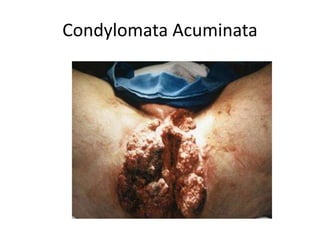
Genital warts, caused by various strains of the human papillomavirus (HPV), are highly contagious and can manifest on genital and extragenital areas. The low-risk HPV types 6 and 11 account for most genital warts, while high-risk types are linked to cancers. Treatment options include topical agents, immune response modifiers, and ablative therapies, with recent advancements in preventive vaccines like Gardasil.