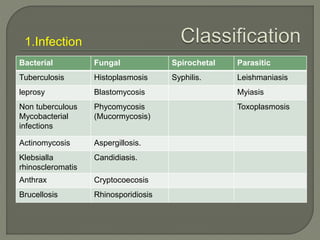
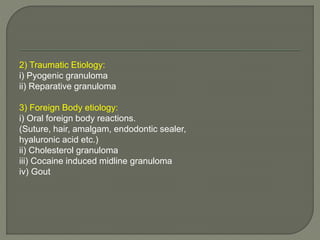
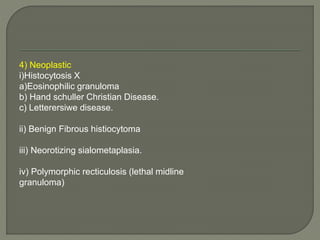
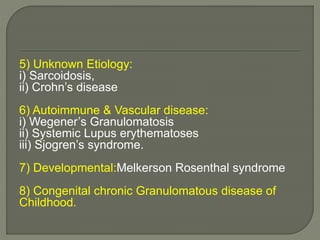
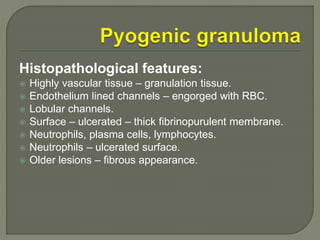
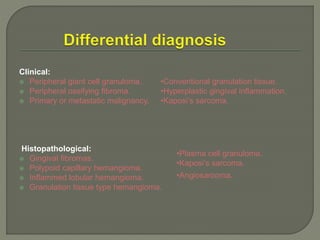
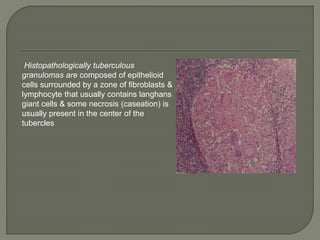
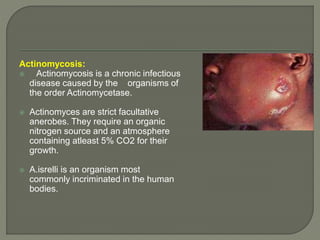
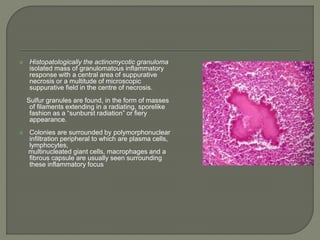
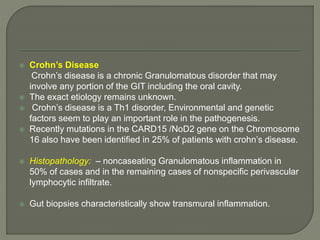
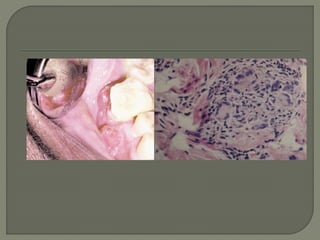
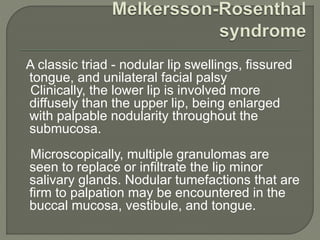
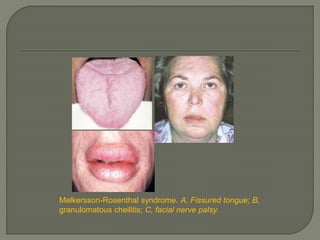
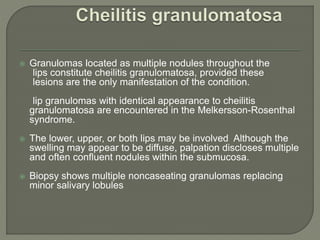
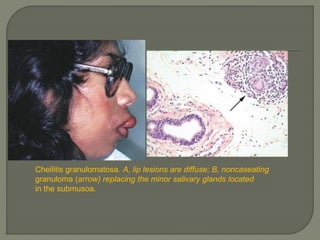
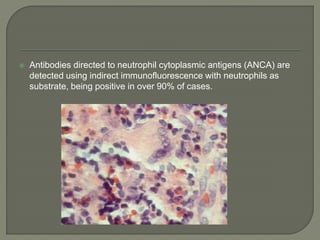
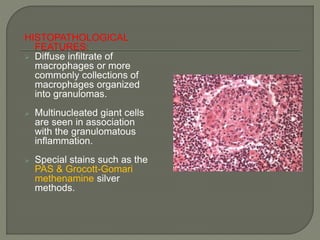
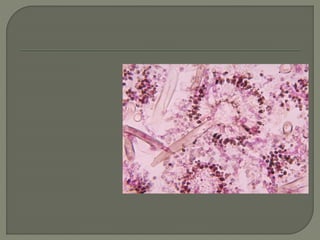
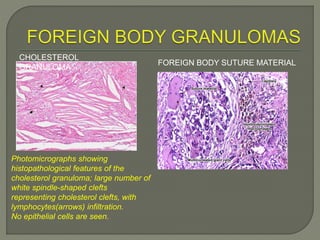
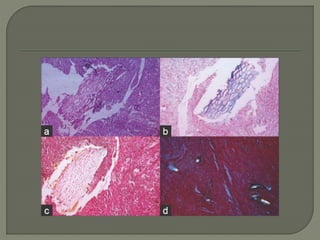
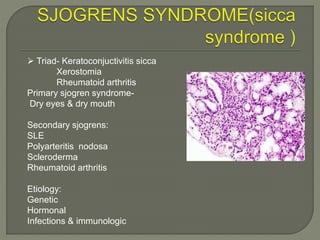
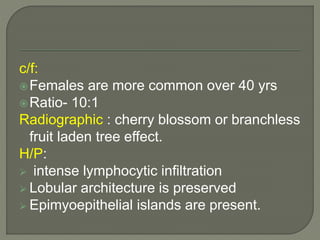
This document discusses oral granulomatous diseases. It defines granulomas as chronic inflammatory lesions composed of macrophages, epithelioid cells, and multinucleated giant cells. Granulomas form in response to infection, foreign bodies, or immune responses. The document classifies granulomatous diseases including those of infectious etiology like tuberculosis, leprosy, and actinomycosis. It describes the histopathological features of granulomas and provides photomicrographs. Specific conditions like sarcoidosis, Crohn's disease, and Melkersson-Rosenthal syndrome are also summarized.