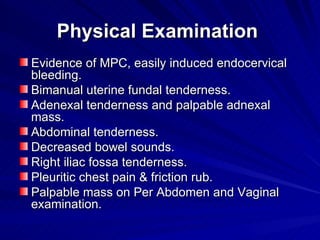
Pelvic Inflammatory Disease (PID) is an infection and inflammation of the upper female genital tract involving the fallopian tubes and ovaries. It is usually caused by ascending infection from the cervix or vagina, often due to bacteria like Neisseria gonorrhoeae or Chlamydia trachomatis. Risk factors include multiple sexual partners and IUD use. Symptoms include lower abdominal pain and tenderness. Diagnosis involves clinical examination and testing for sexually transmitted infections. Treatment aims to cover common causative bacteria with antibiotic regimens. Without treatment, PID can cause long-term complications like infertility or ectopic pregnancy.