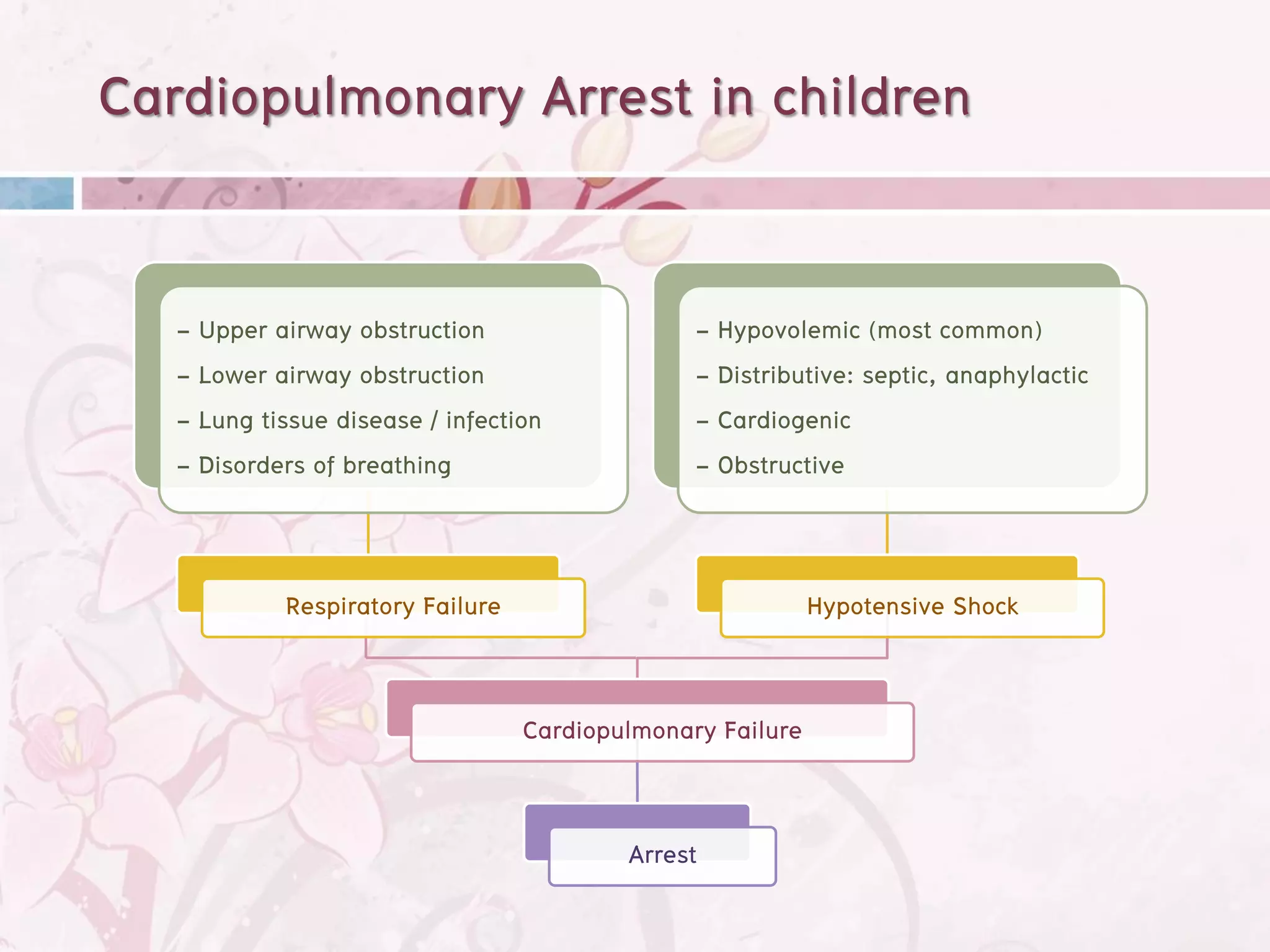
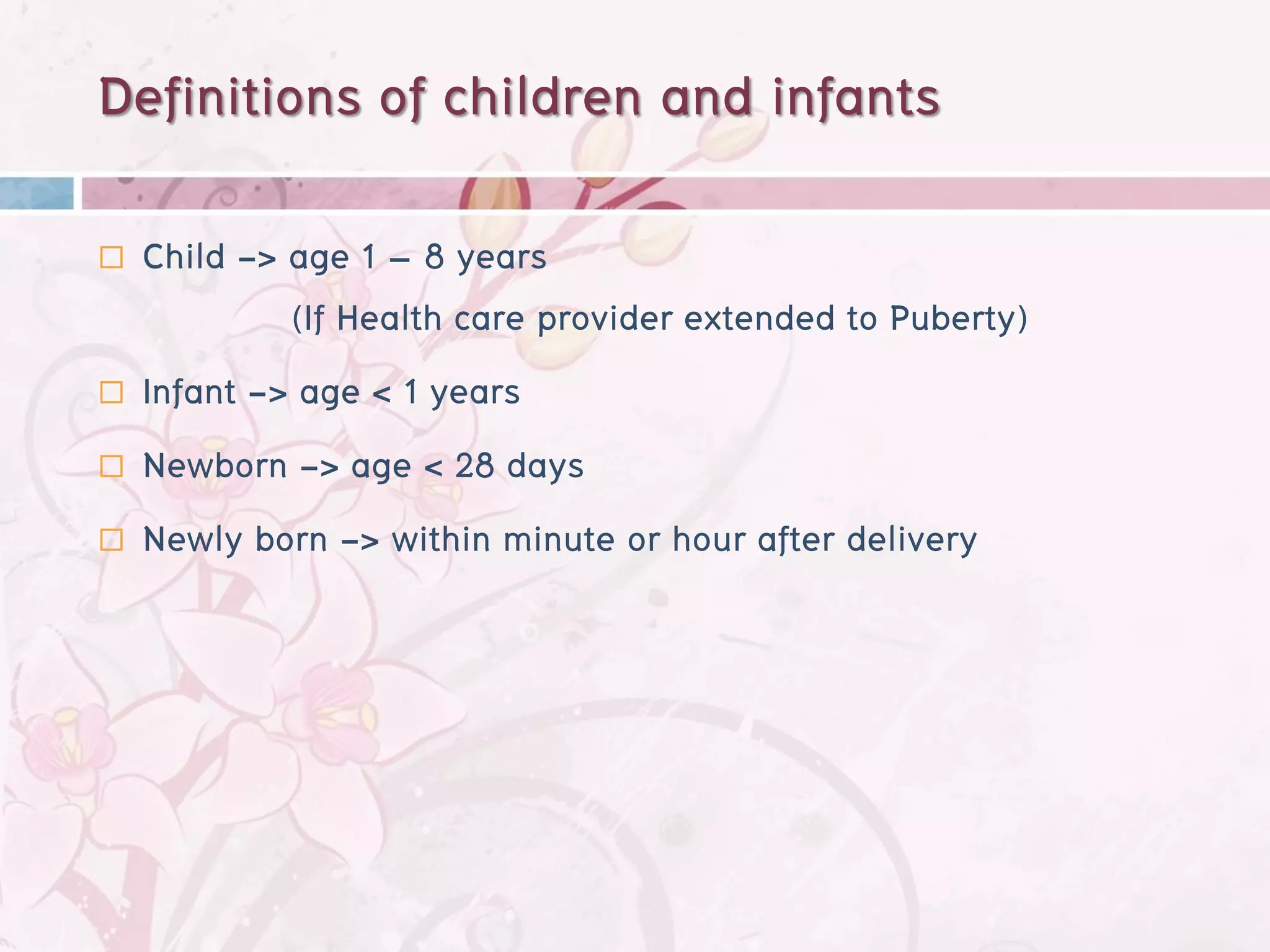
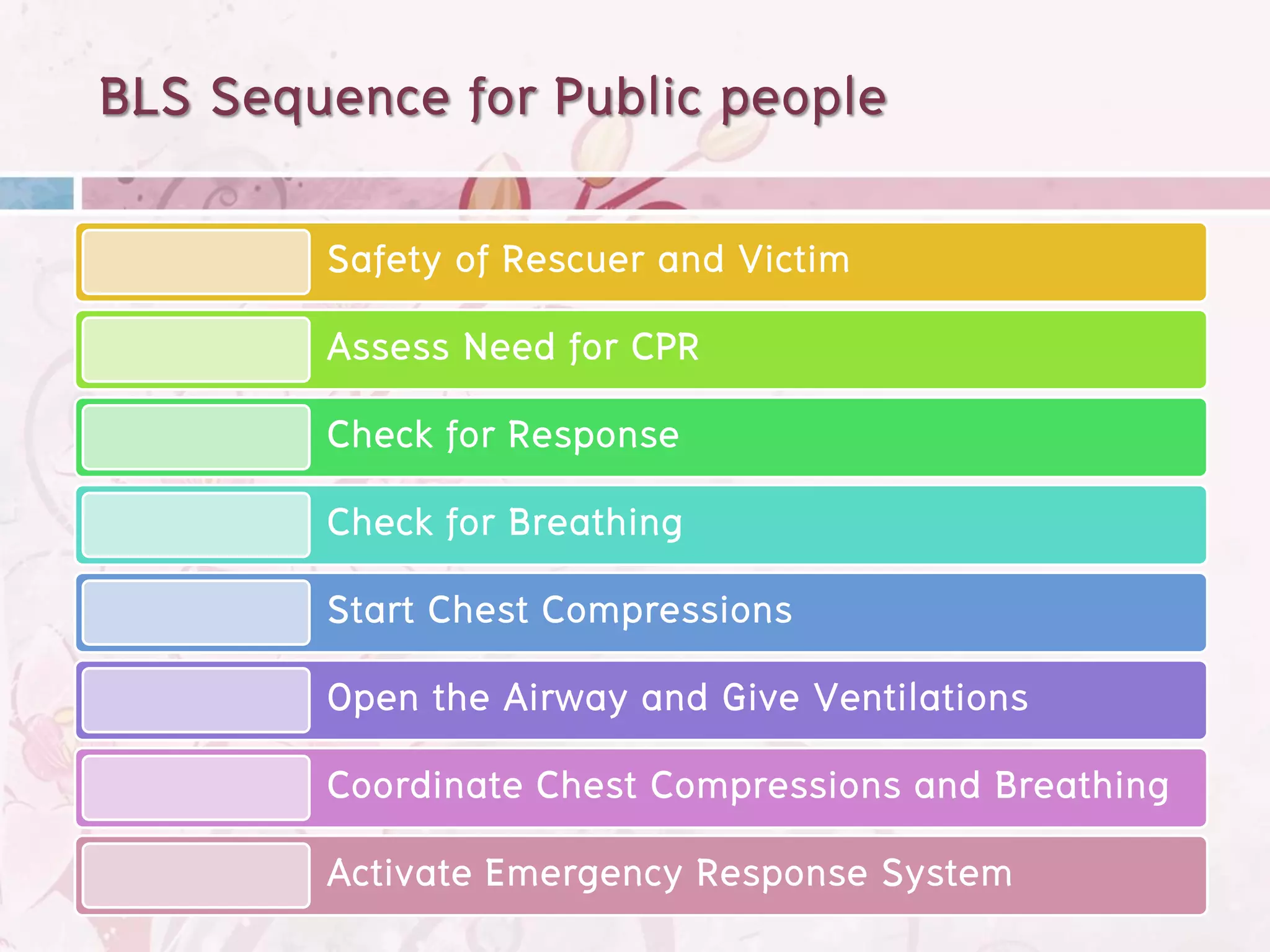
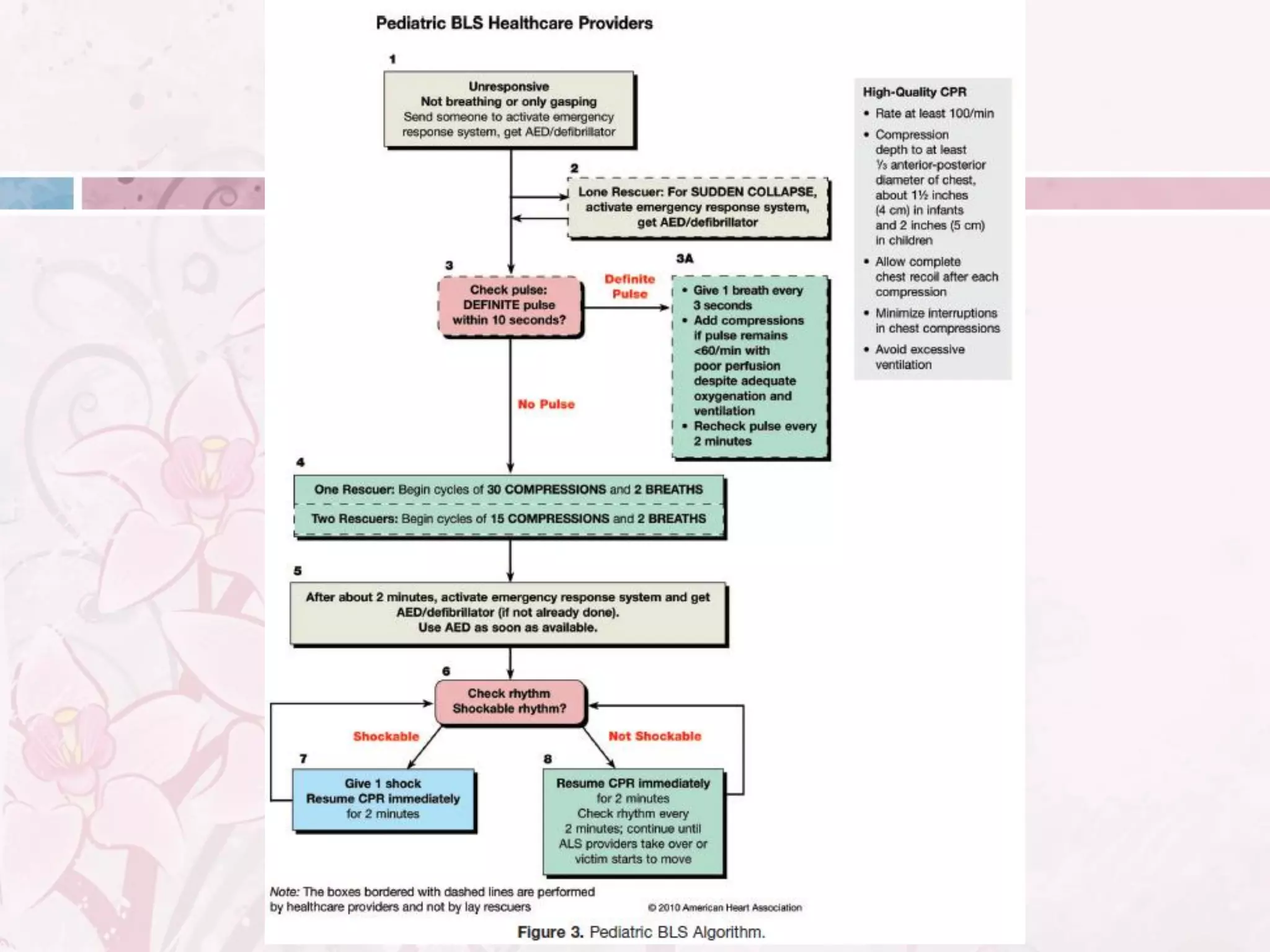
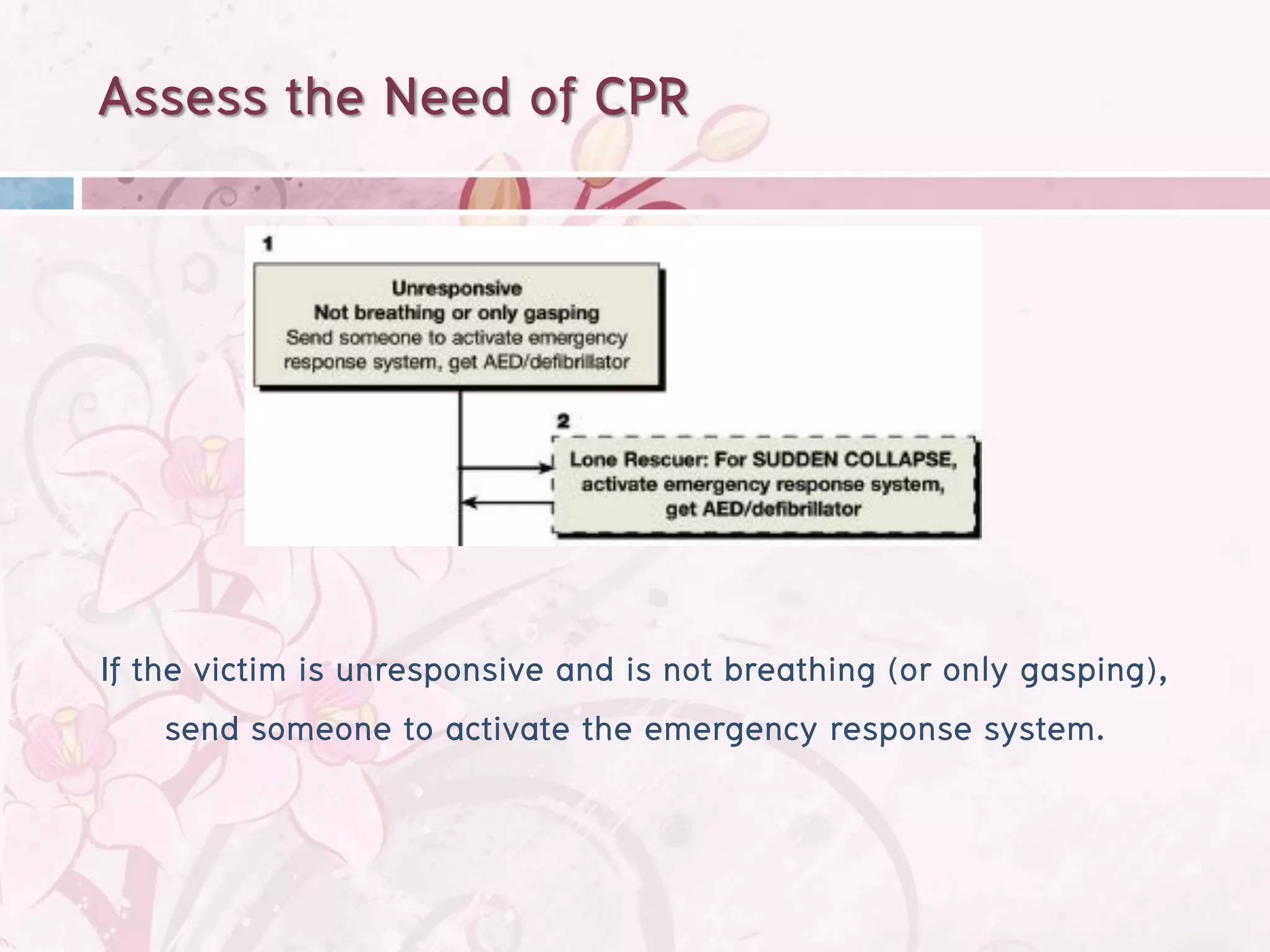
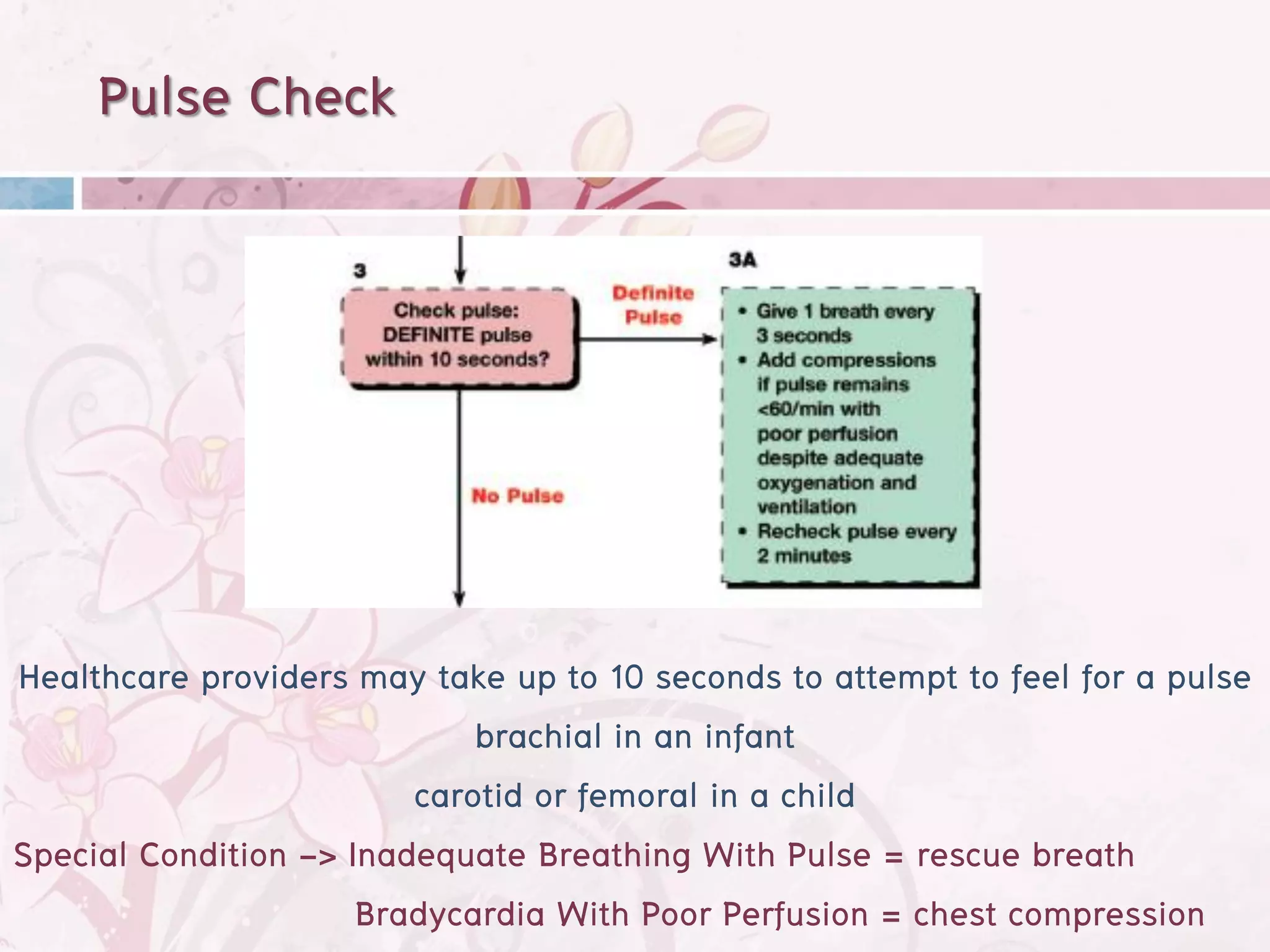
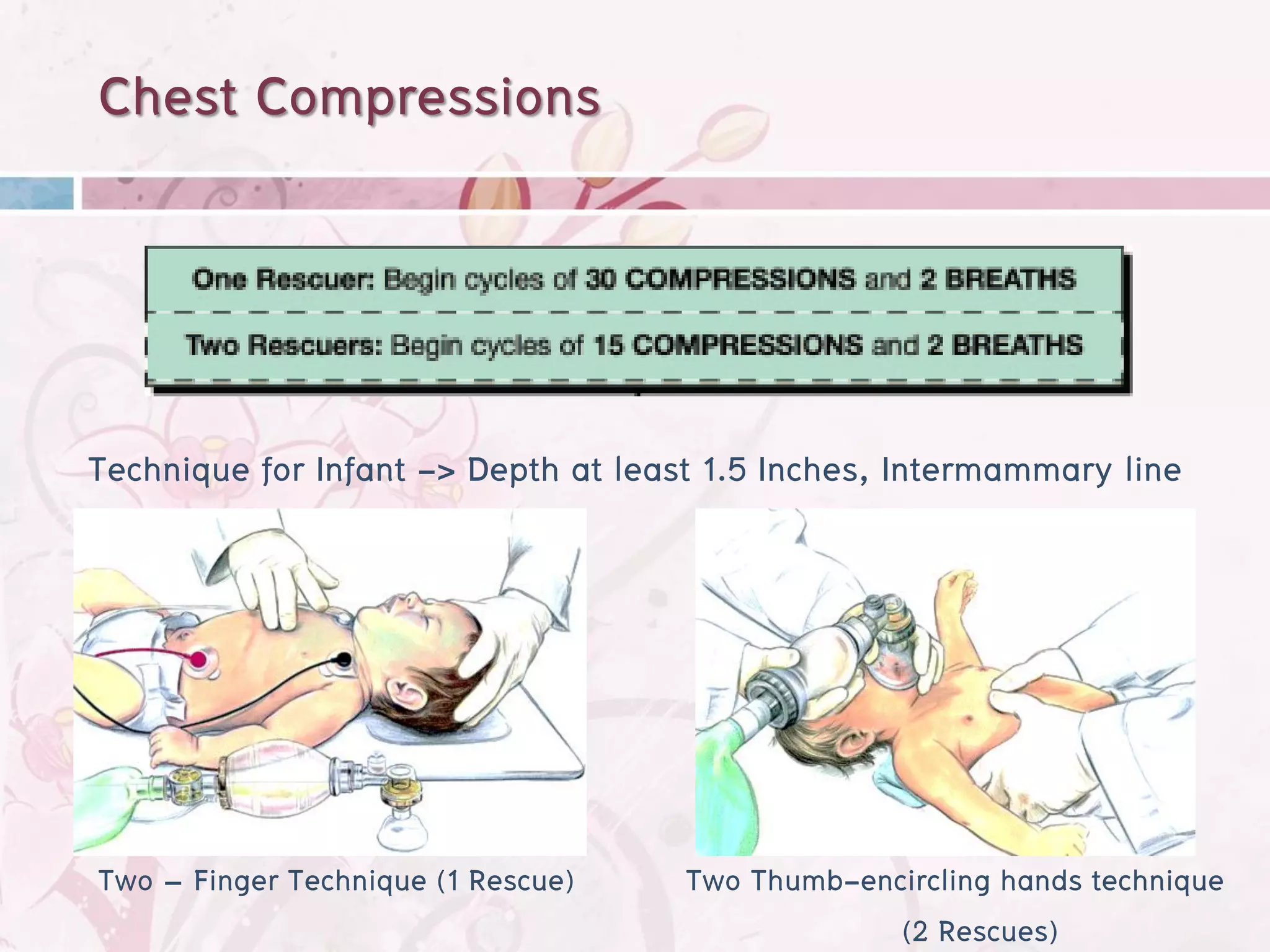
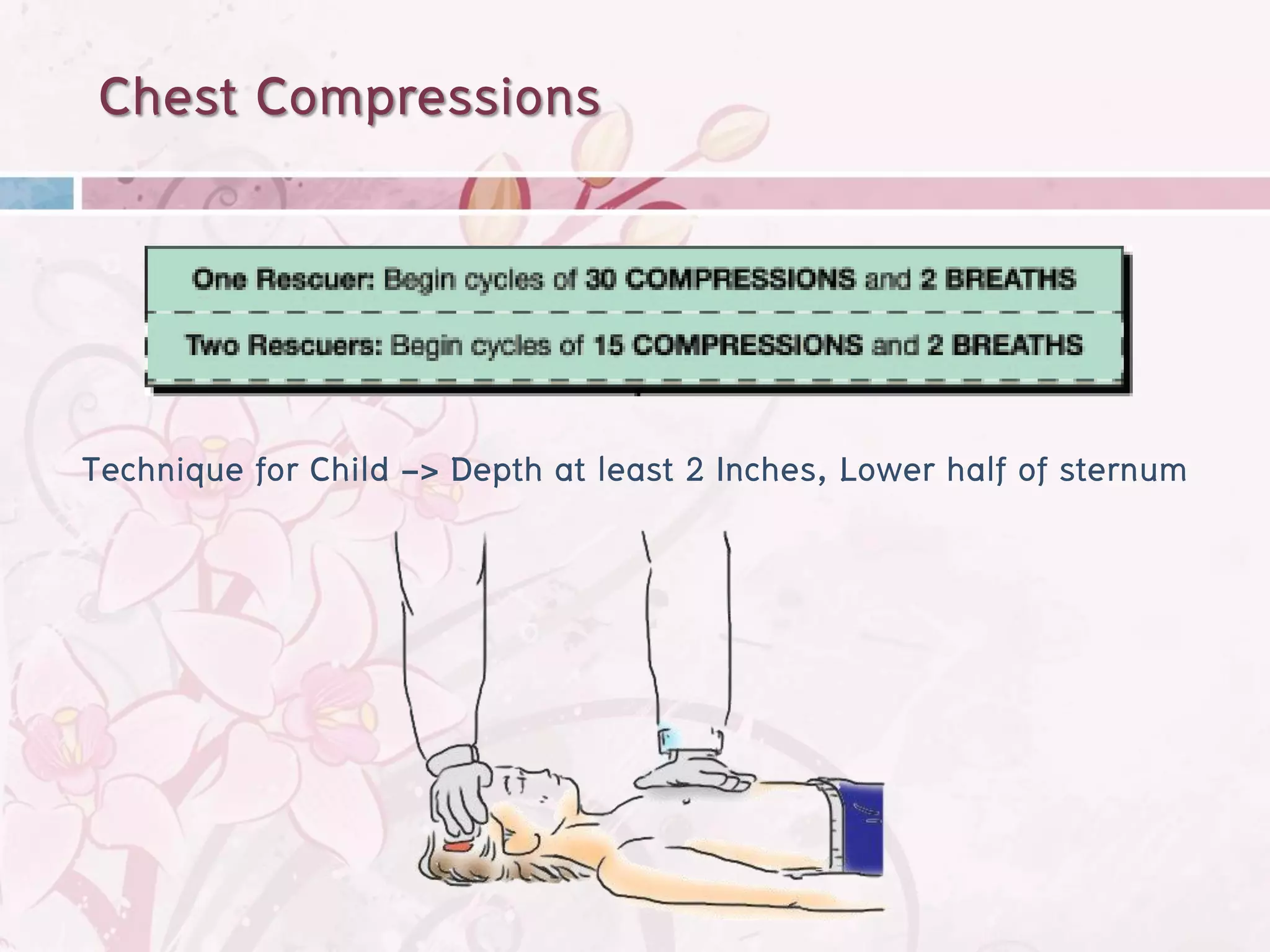
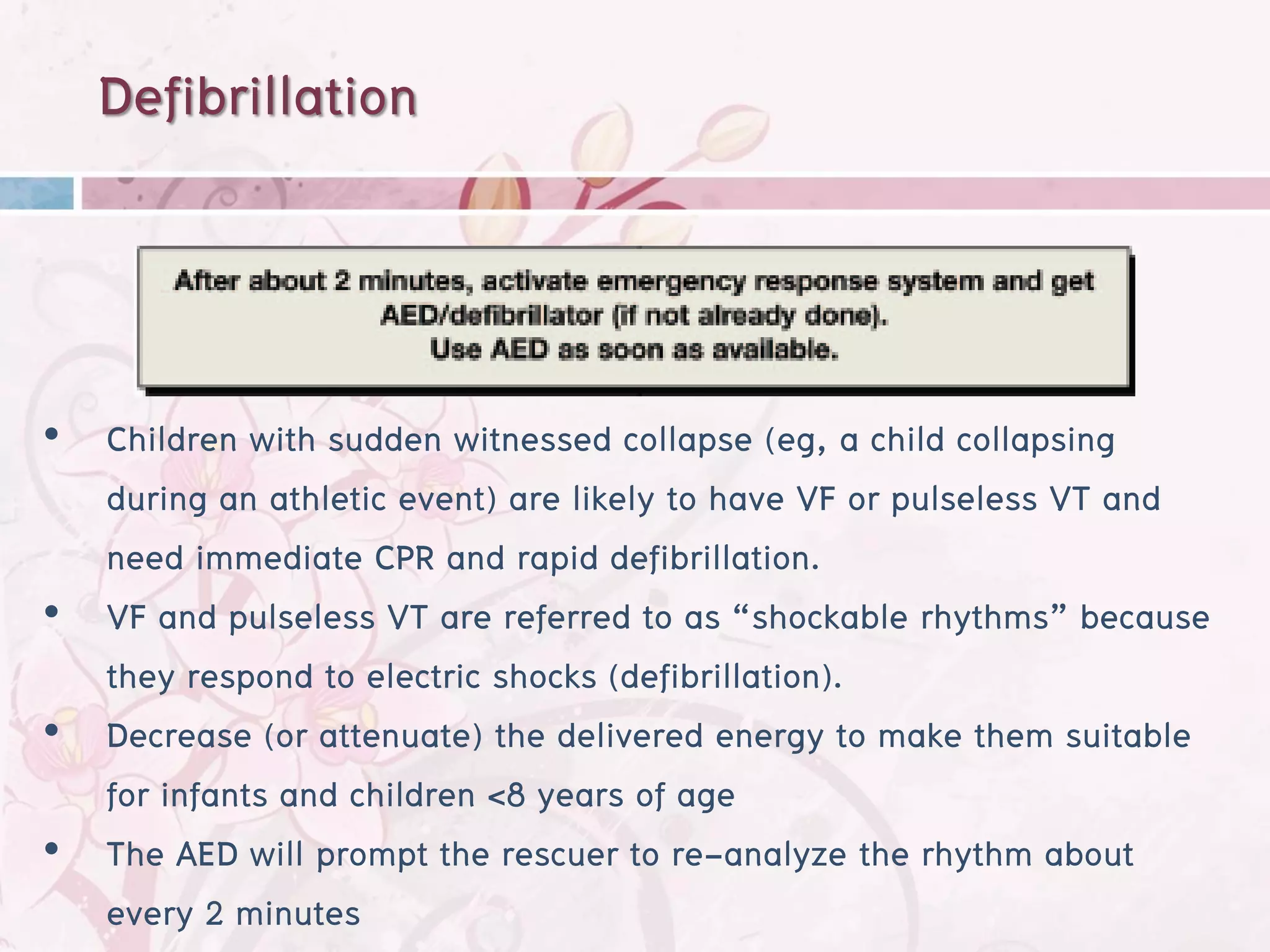
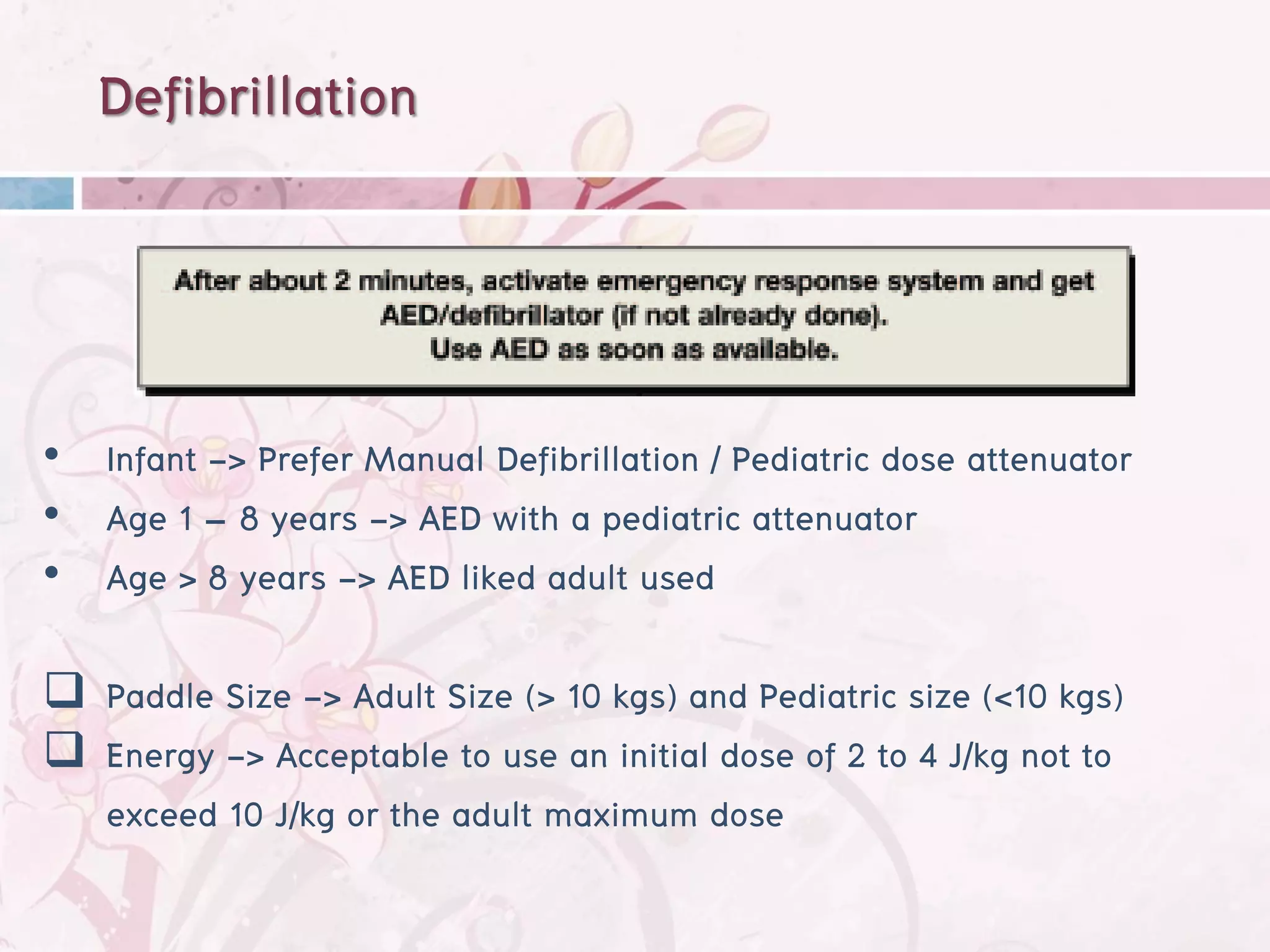
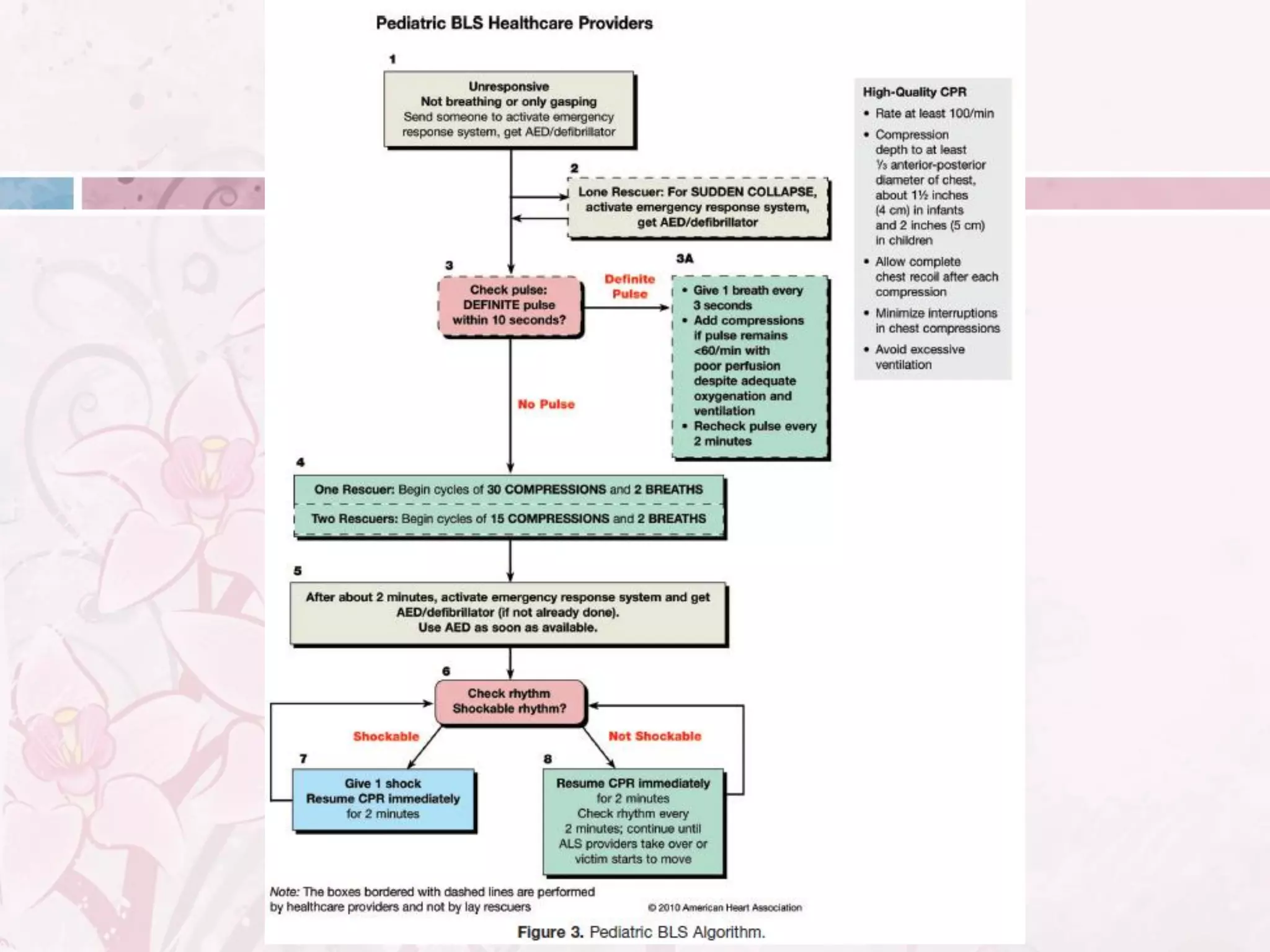
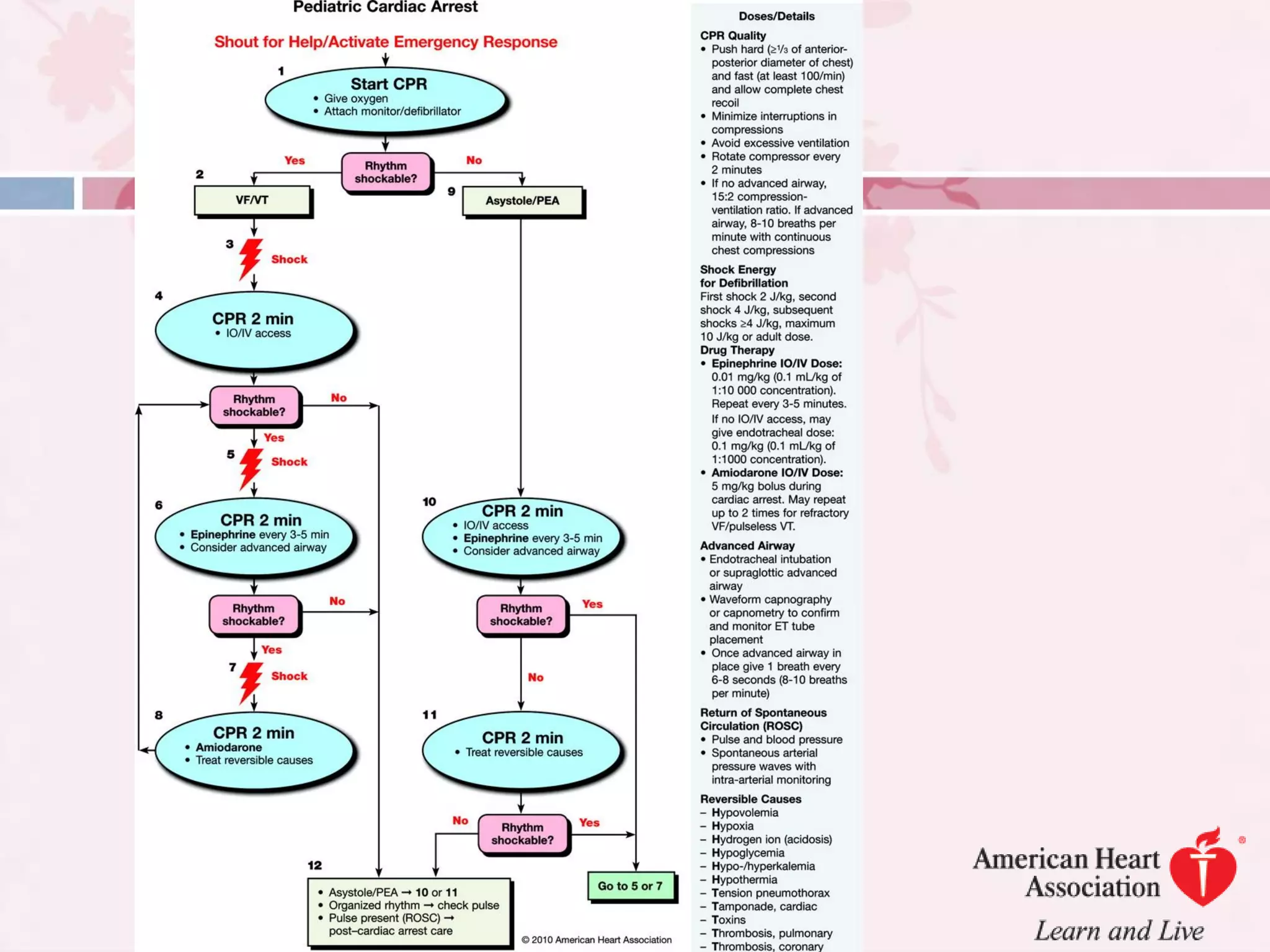
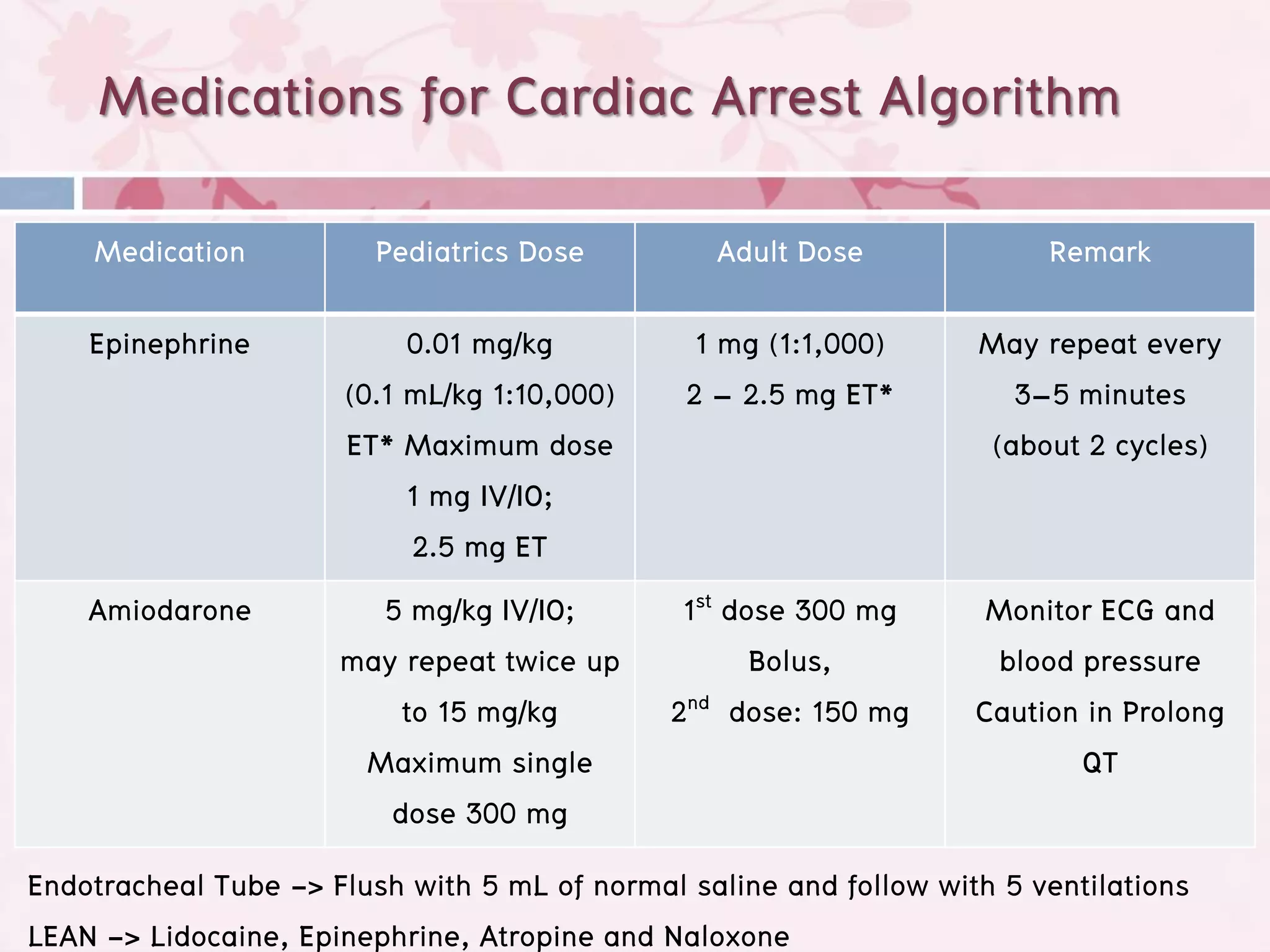
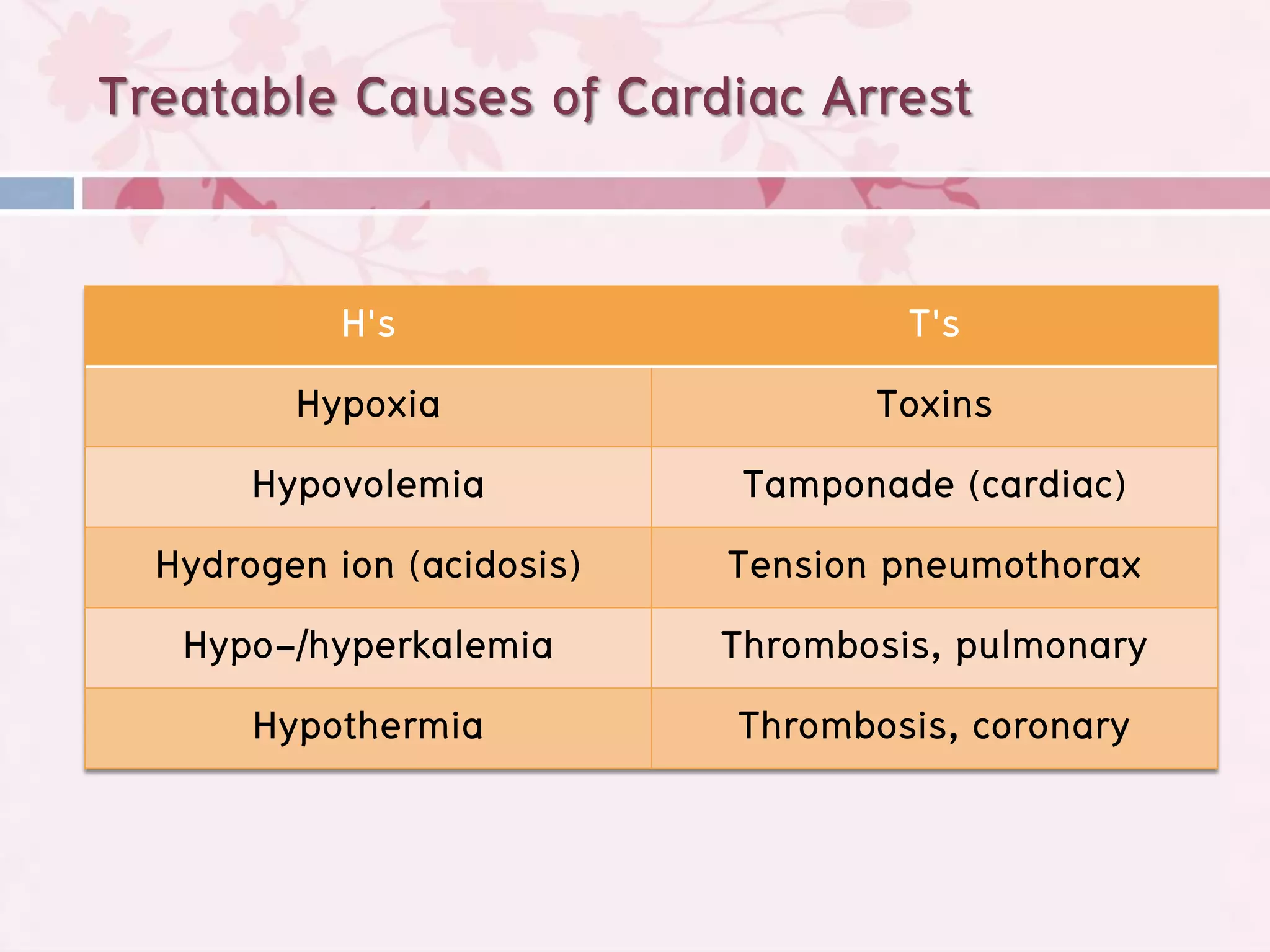
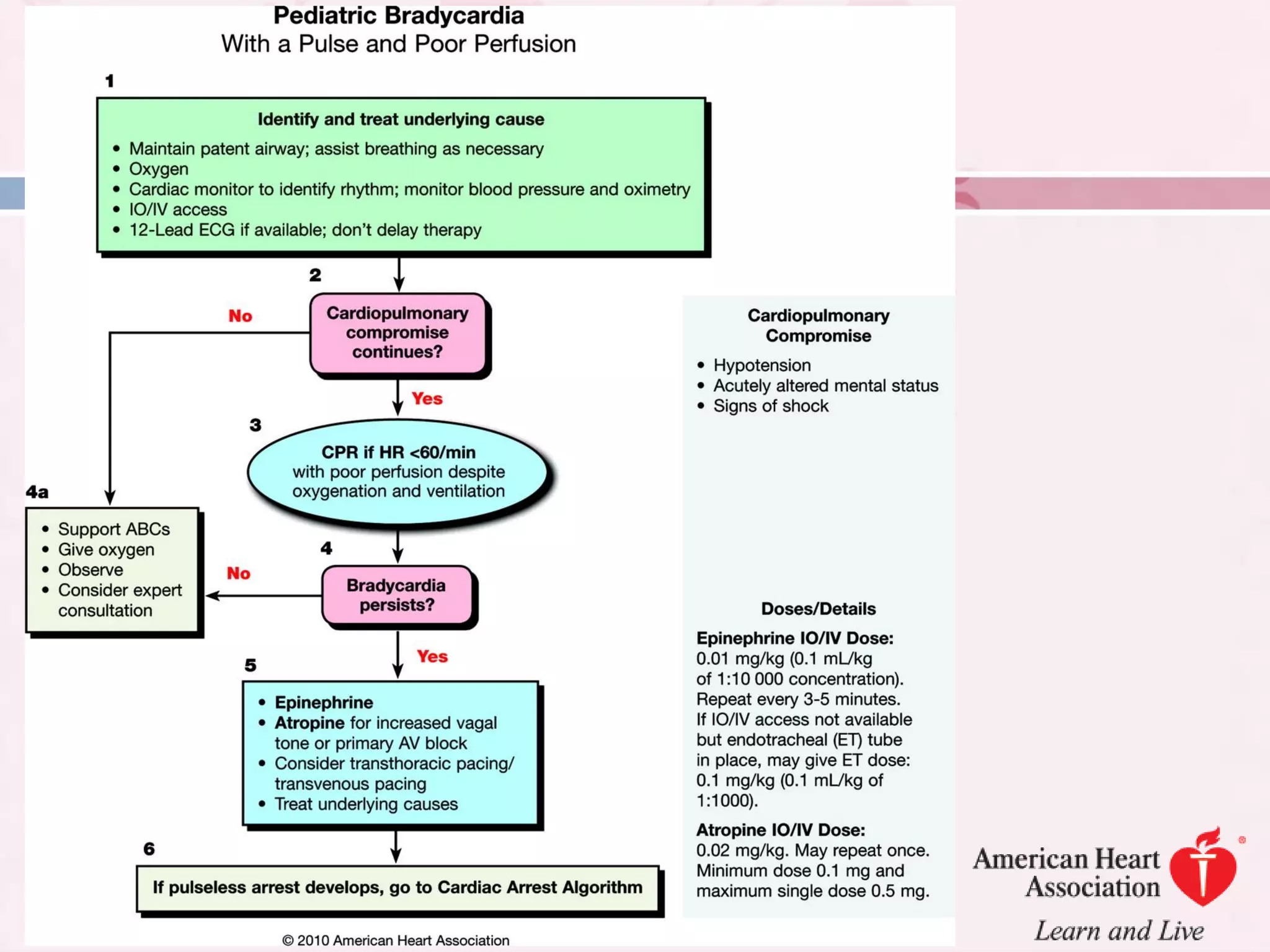
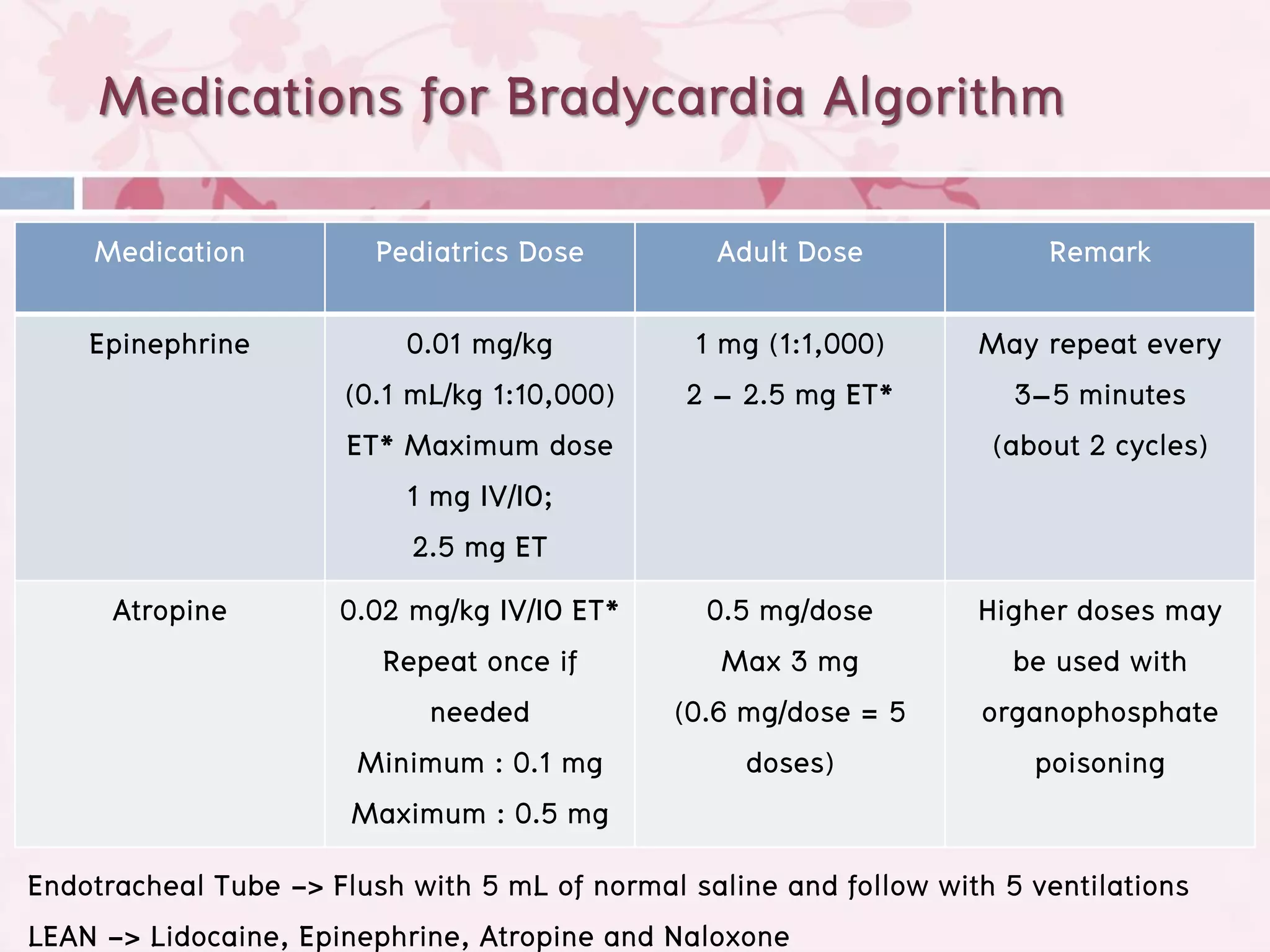
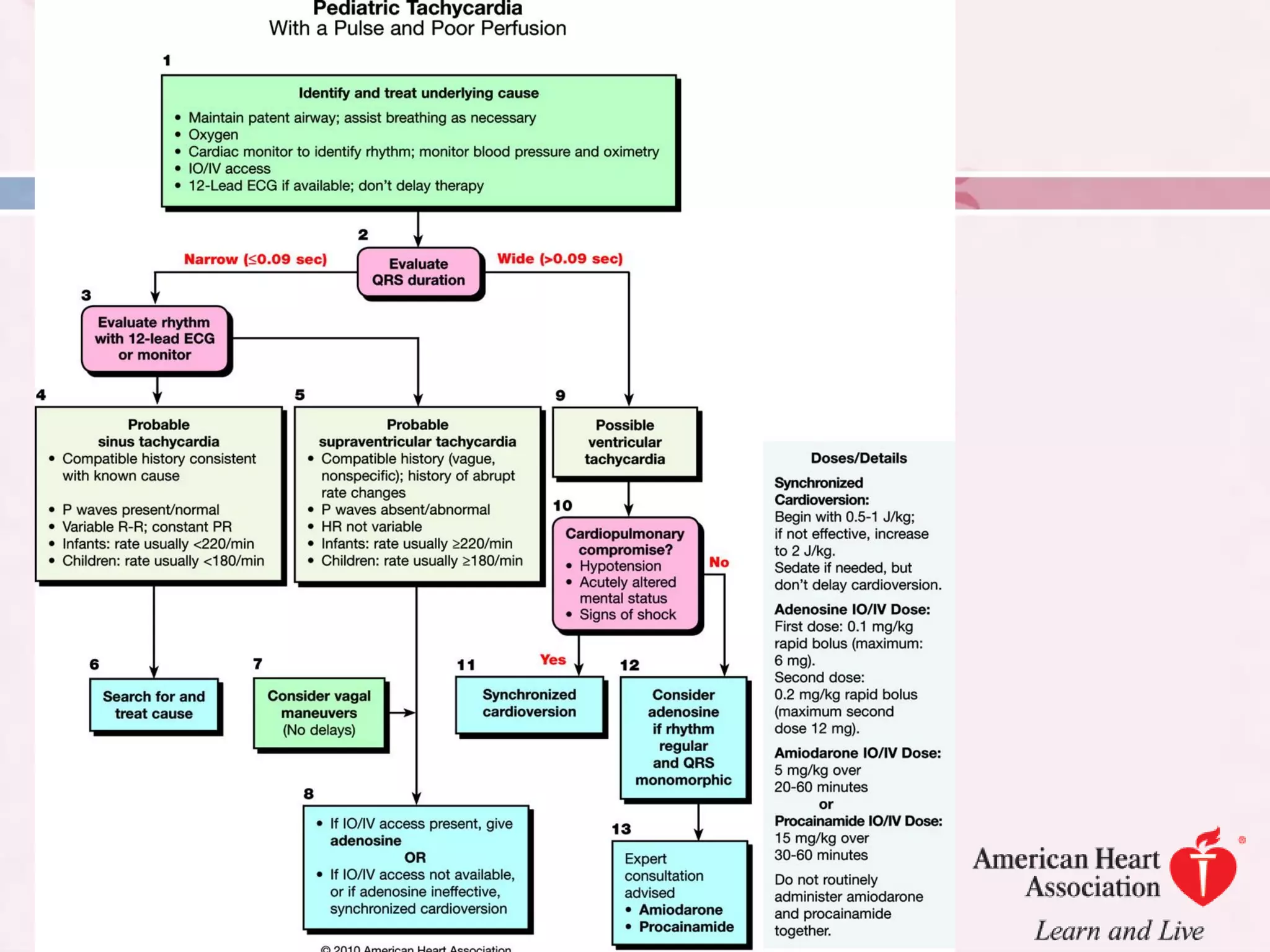
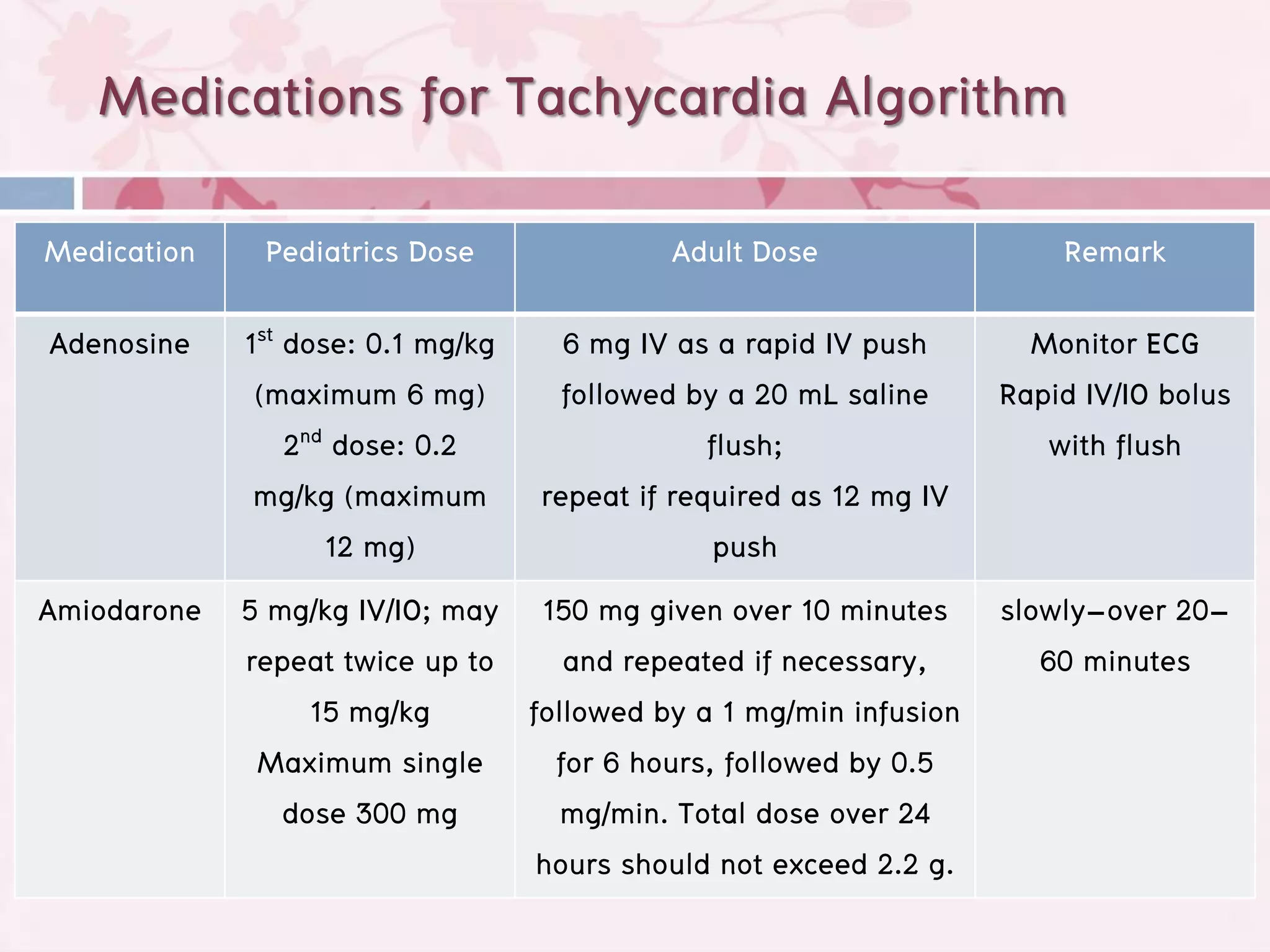
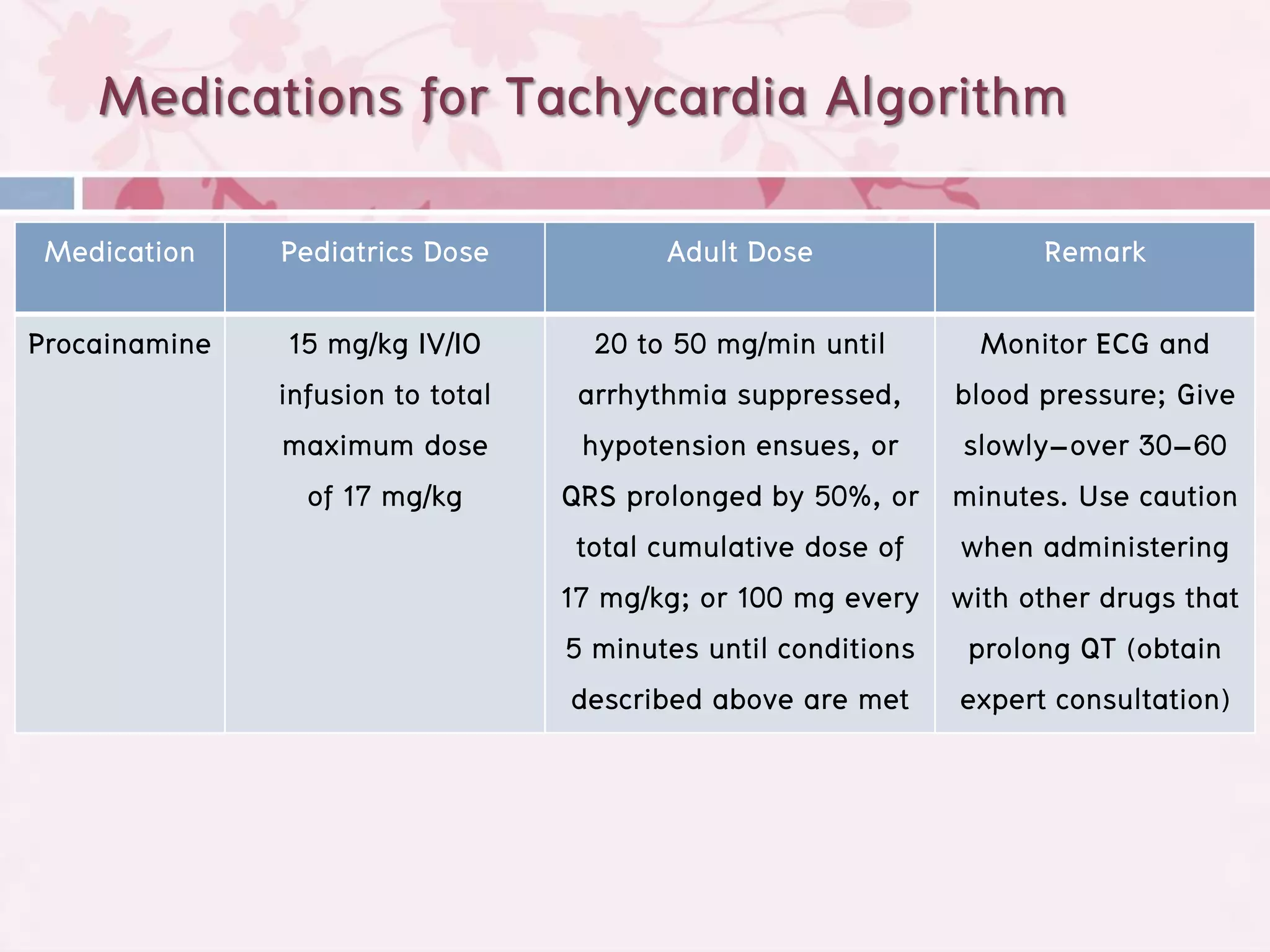
This document summarizes pediatric basic and advanced life support. It outlines 5 key steps for pediatric basic life support: 1) prevent cardiac arrest, 2) early CPR, 3) prompt emergency response, 4) rapid pediatric advanced life support, and 5) integrated post-cardiac arrest care. Common causes of cardiac arrest in children include respiratory issues, burns, drowning, dysrhythmias, foreign body aspiration, gastroenteritis, sepsis, seizures, and trauma. The document also provides details on assessments, CPR techniques, airway management, defibrillation, and medications for cardiac arrest, bradycardia, and tachycardia in pediatric patients.