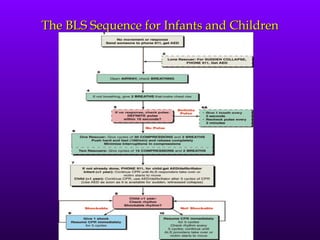
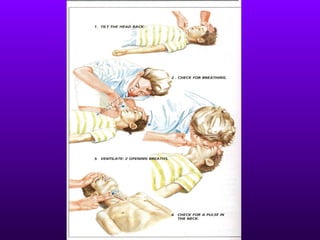
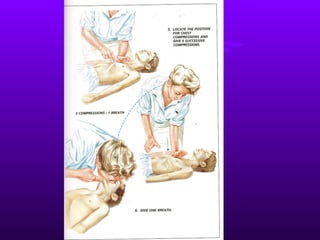
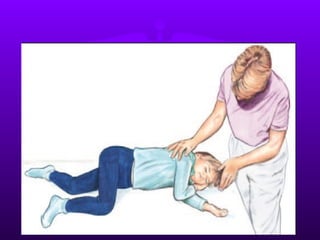
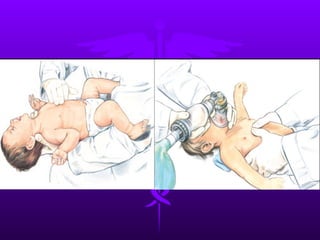
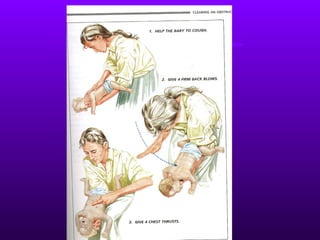
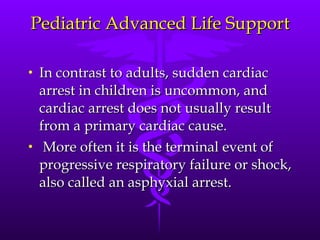
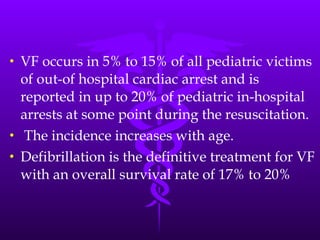
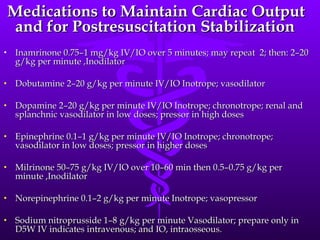
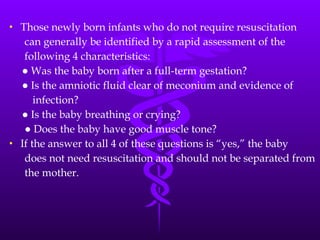
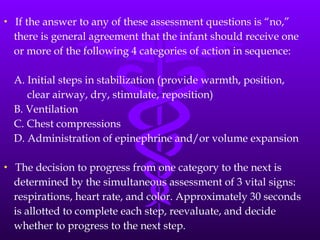
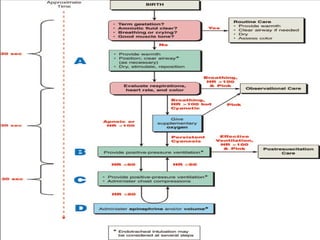
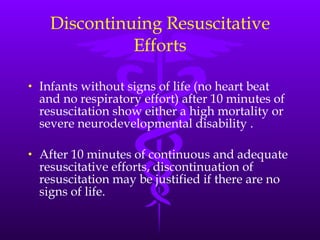
The document discusses pediatric resuscitation, including the chain of survival, causes of cardiac arrest in children, basic life support sequences, advanced life support, and neonatal resuscitation guidelines. It notes that rapid bystander CPR and access to emergency services are key to survival for children experiencing cardiac arrest. For newborns, the document outlines assessing respiration, heart rate, muscle tone and gestational age to determine if resuscitation is required, with steps including warming, clearing airways, and ventilation or compressions if needed. Endotracheal intubation may be used during resuscitation of newborns when other methods are ineffective or for procedures like suctioning meconium.