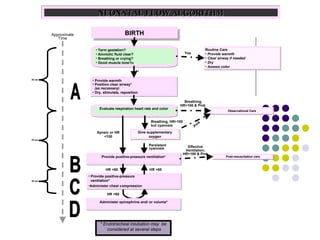
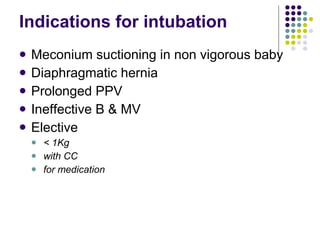
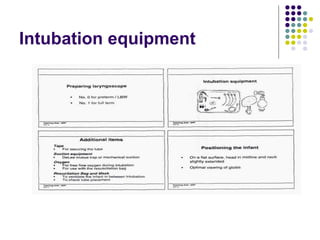
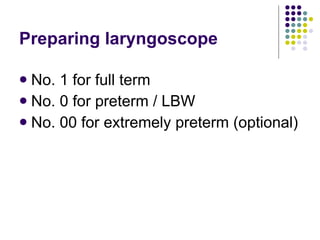
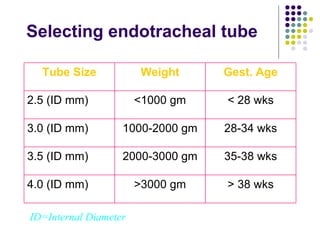
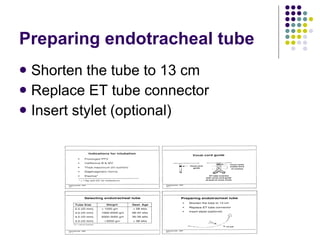
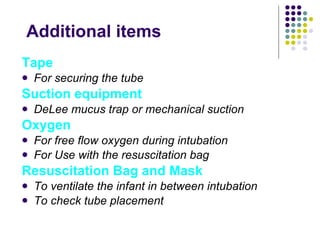
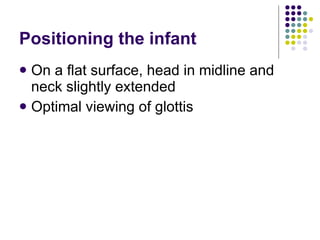
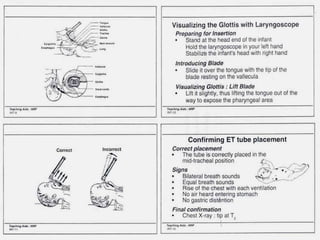
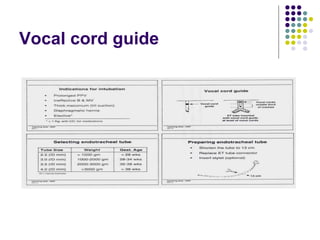
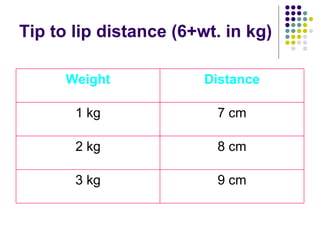
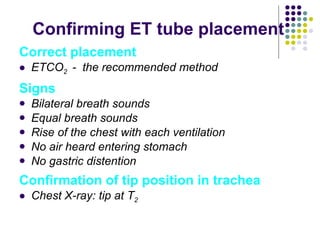
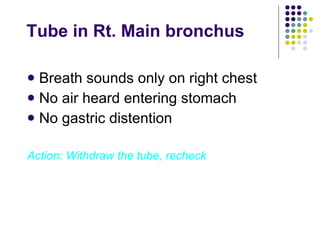
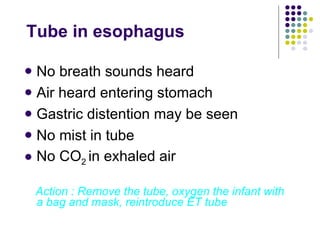
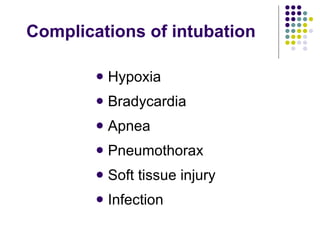
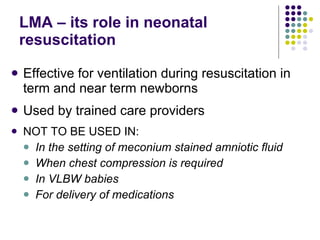
This document provides an algorithm and guidelines for endotracheal intubation in neonates. It outlines the indications for intubation, necessary equipment, proper technique including positioning, visualizing the glottis, confirming tube placement, actions after intubation, and complications to minimize. Key steps include preparing the laryngoscope and selecting the appropriately sized endotracheal tube based on gestational age and weight. Placement is confirmed through bilateral breath sounds, chest rise, and monitoring exhaled carbon dioxide levels.