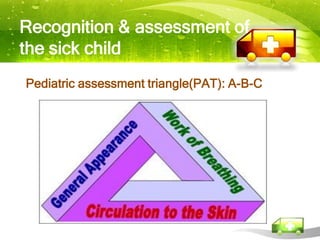
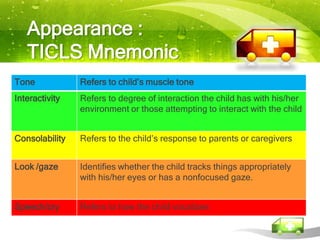
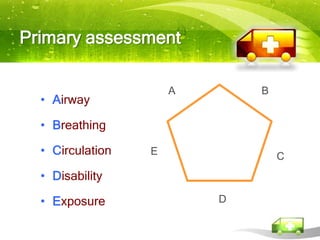
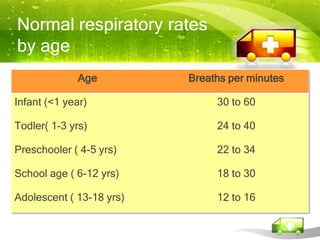
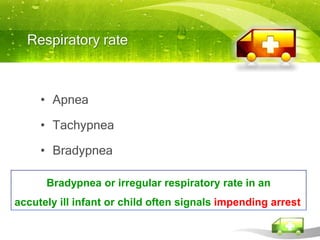
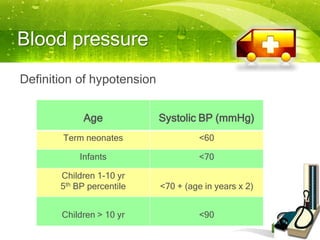
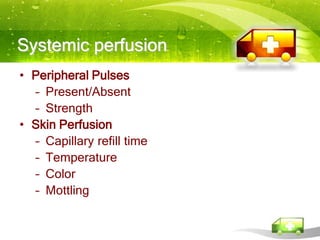
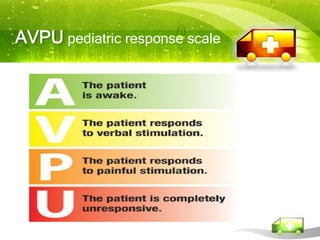
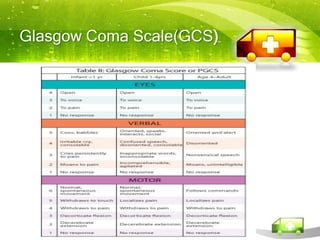
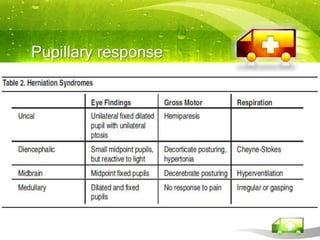
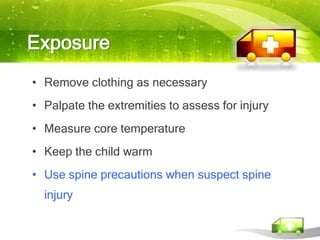
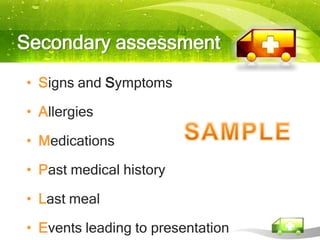
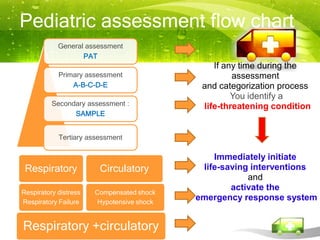
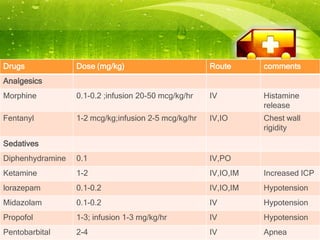
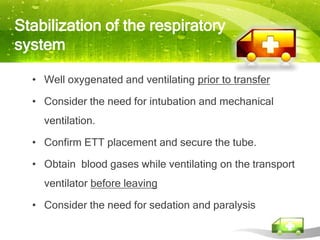
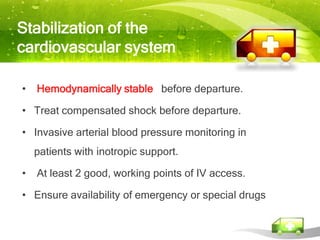
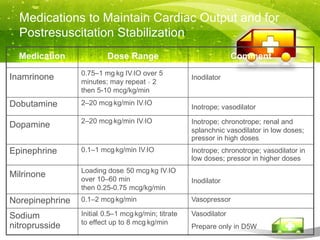
Pediatric transport involves stabilizing critically ill children and continuing critical care therapies en route. The transport team conducts a thorough assessment using standardized approaches like the pediatric assessment triangle and ABCDE model. Key priorities are stabilizing the airway, breathing, circulation, neurological status and managing pain and anxiety. Important equipment includes ventilators, infusion pumps, suction, monitoring and temperature regulation devices designed for portability and reliability during transport. Proper preparation is essential to minimize risks and continue care seamlessly between facilities.