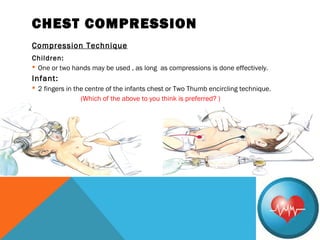
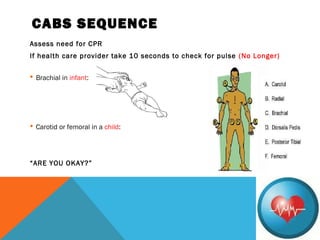
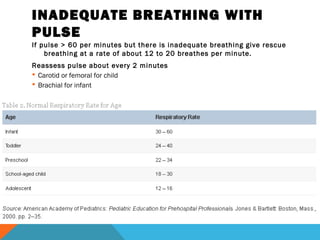
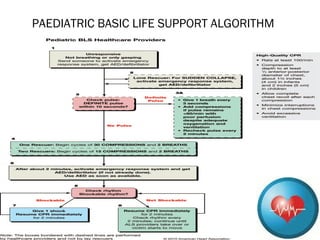
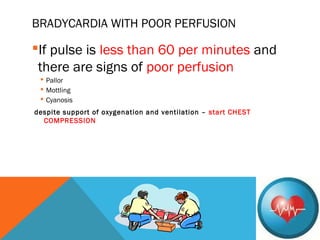
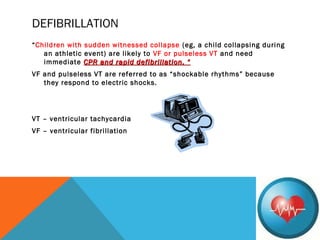
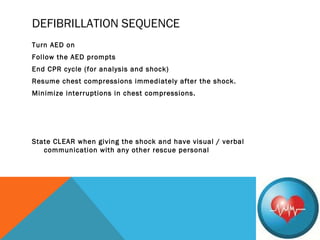
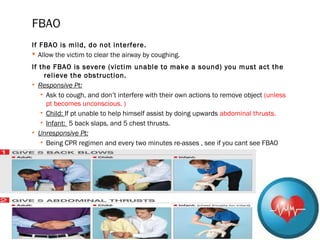
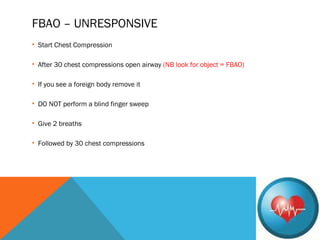
The document outlines Pediatric Basic Life Support (PBLS) guidelines, emphasizing the CAB sequence: chest Compressions, Airway, and Breathing. It details age classifications for BLS, compression techniques, and the importance of timely CPR and defibrillation in cases of cardiac arrest, particularly in children. Additionally, it addresses foreign-body airway obstruction and appropriate responses based on the severity of the obstruction.