PAPILLOEDEMA
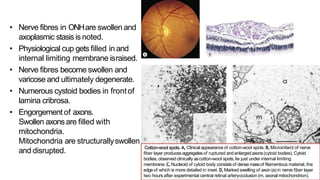
- Oedema of the optic disc caused by increased intracranial pressure. This blocks axoplasmic transport, causing swelling of the optic nerve head.
- Symptoms include blurred vision, visual field defects, and over time potential blindness if not treated.
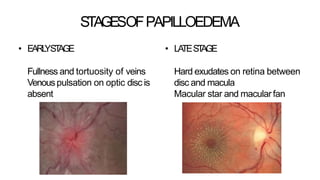
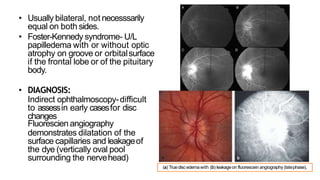
- Diagnosis is made through examination showing blurred disc margins, venous congestion, retinal exudates, and imaging showing disc swelling. Treatment aims to relieve intracranial pressure through surgical or medical means to prevent permanent nerve damage.