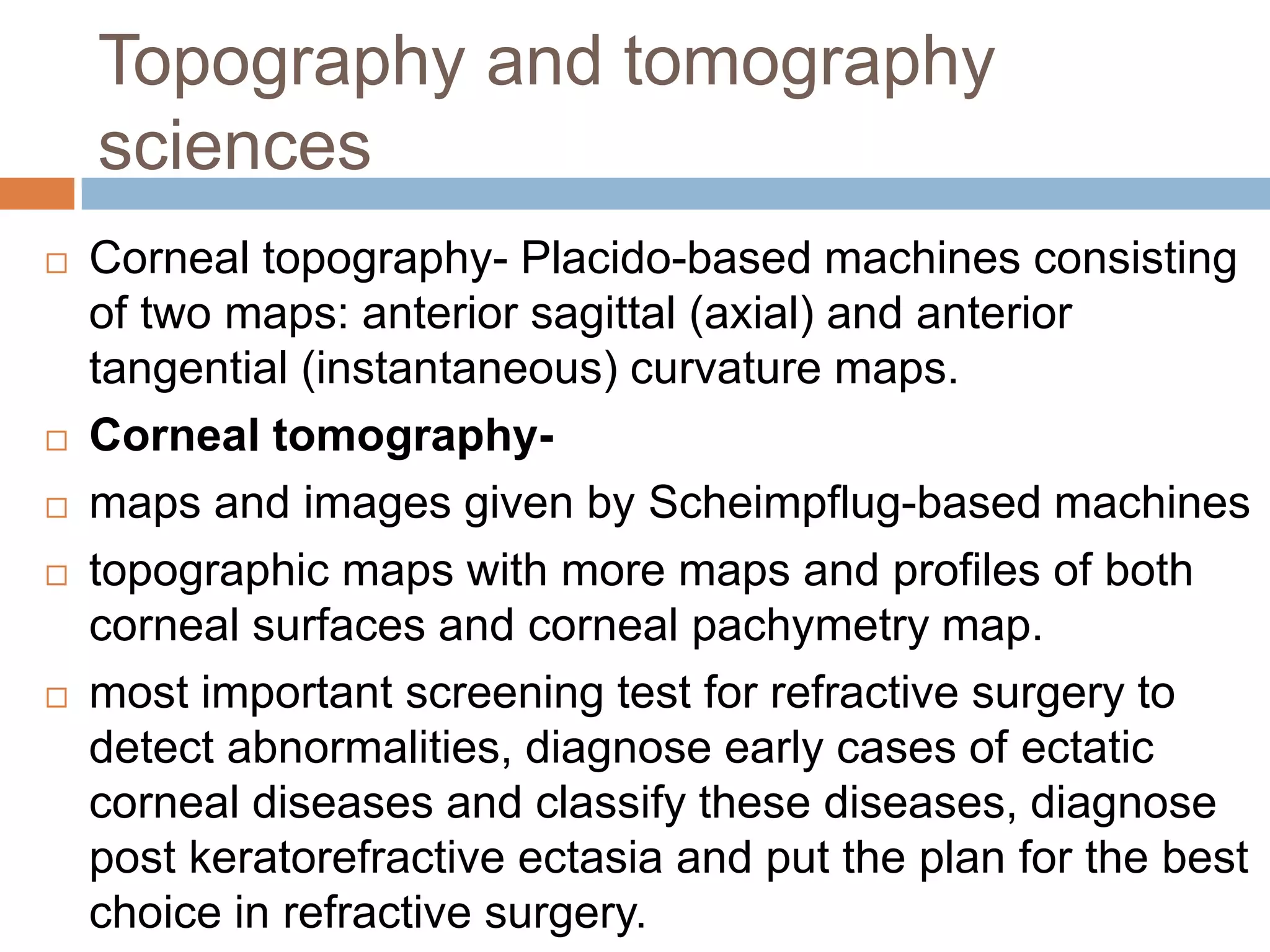
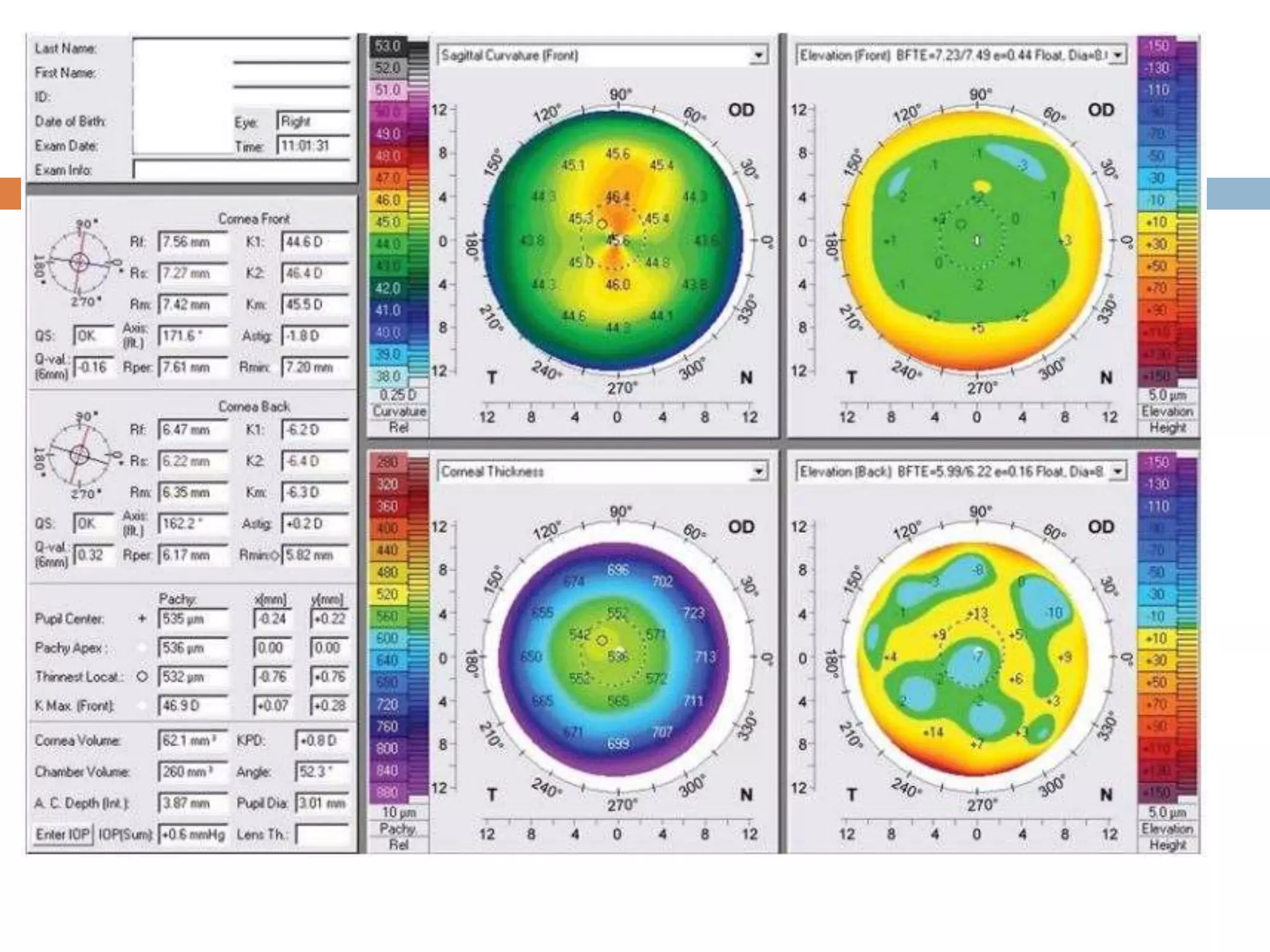
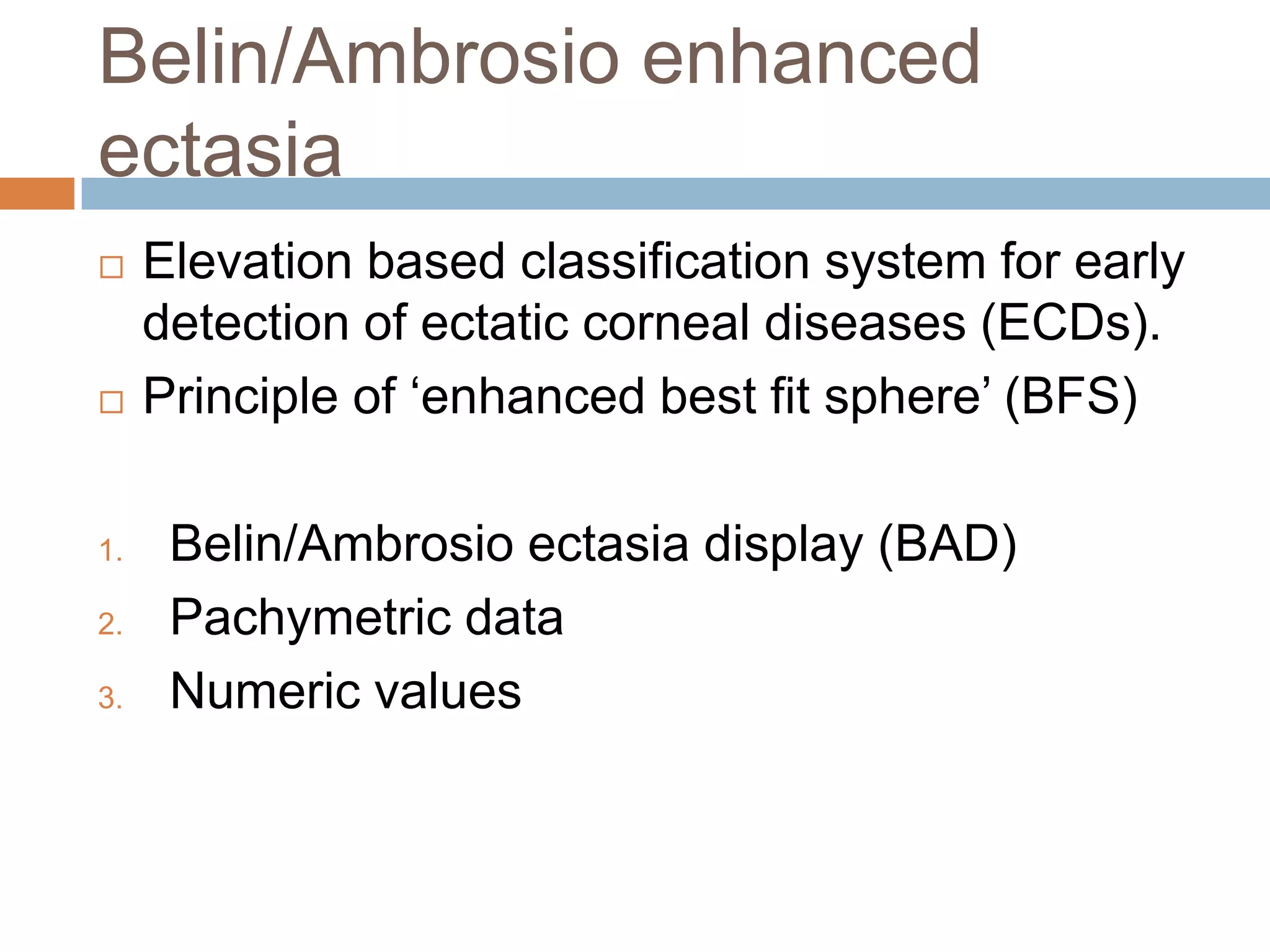
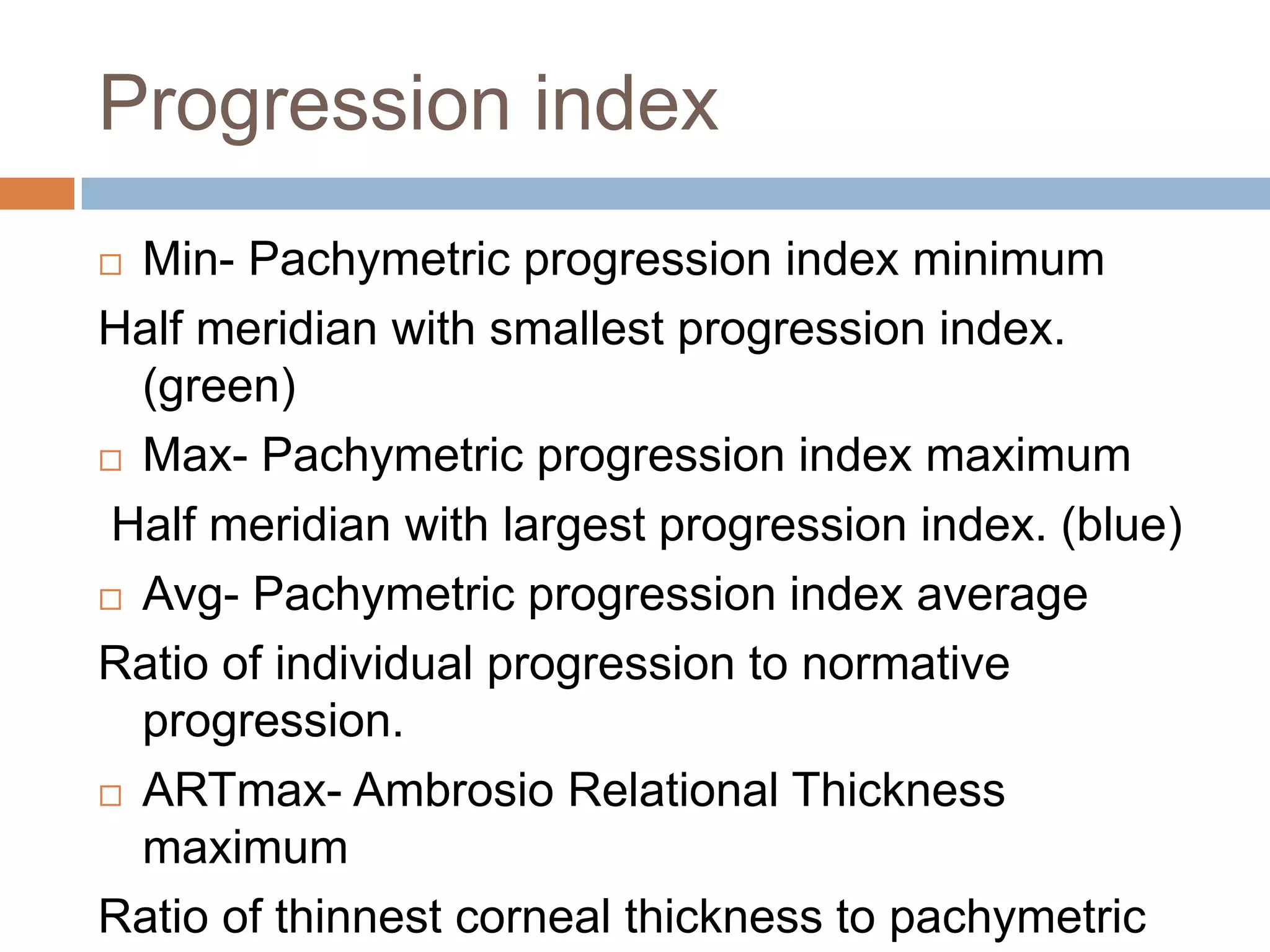
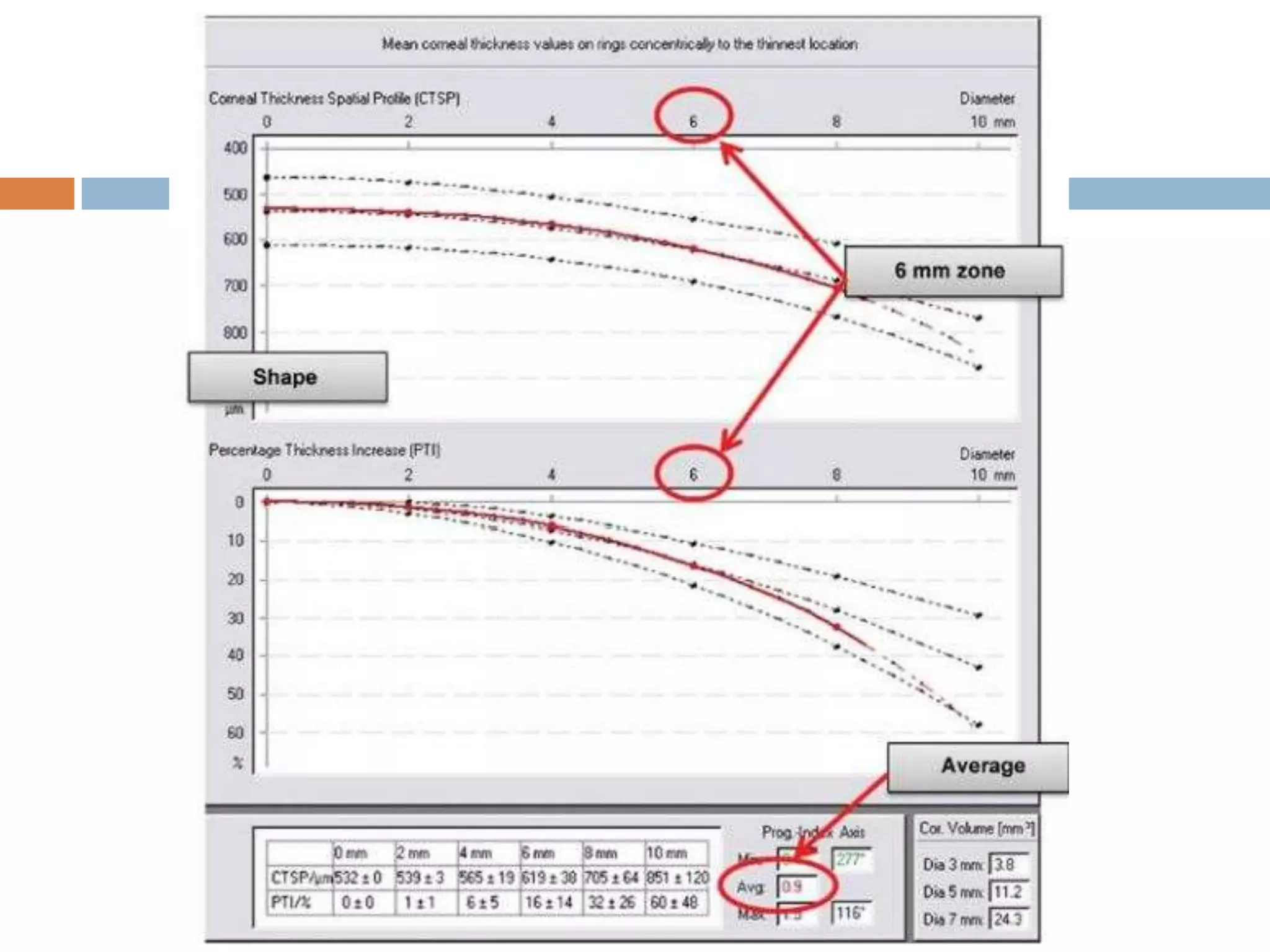
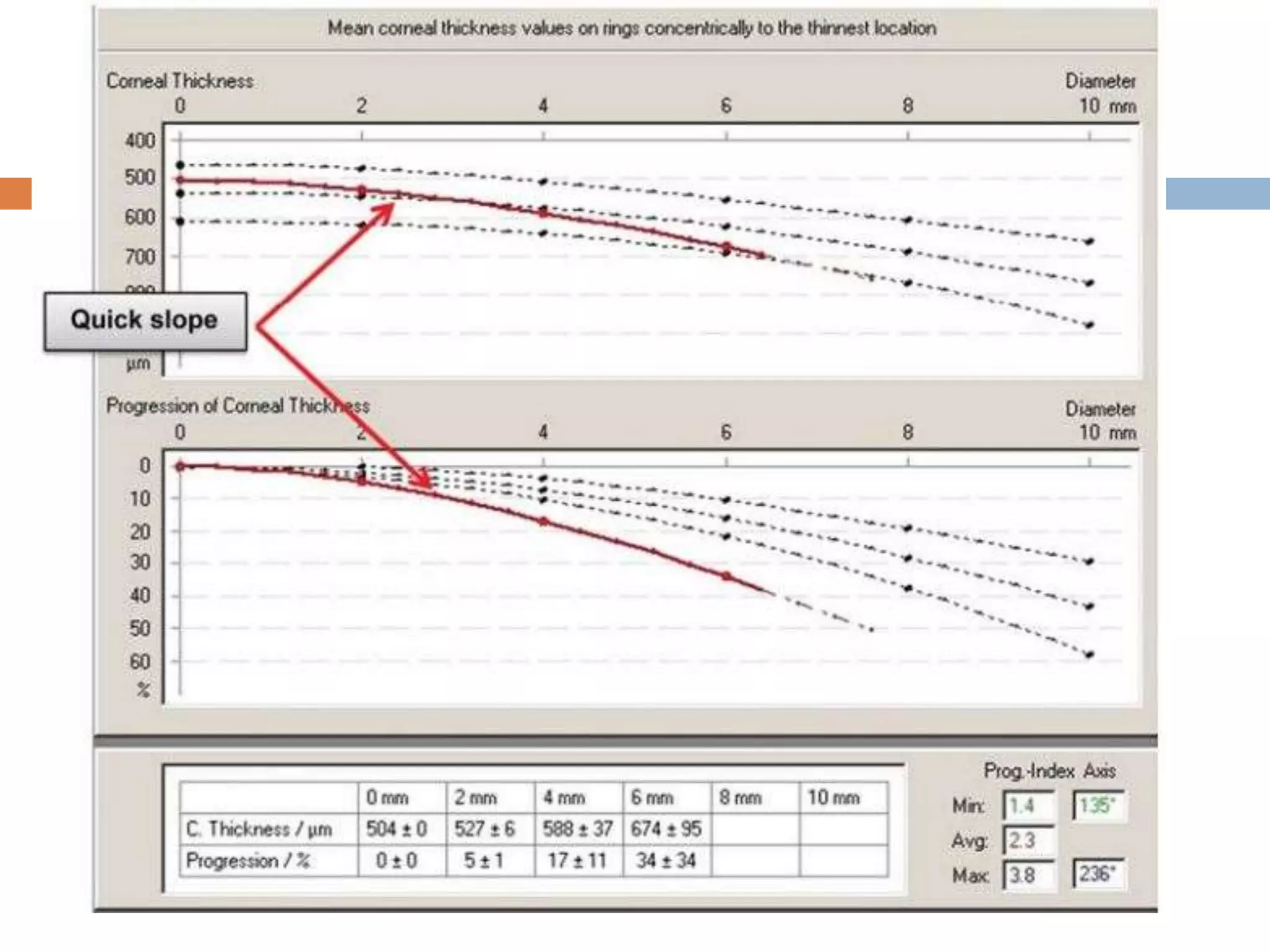
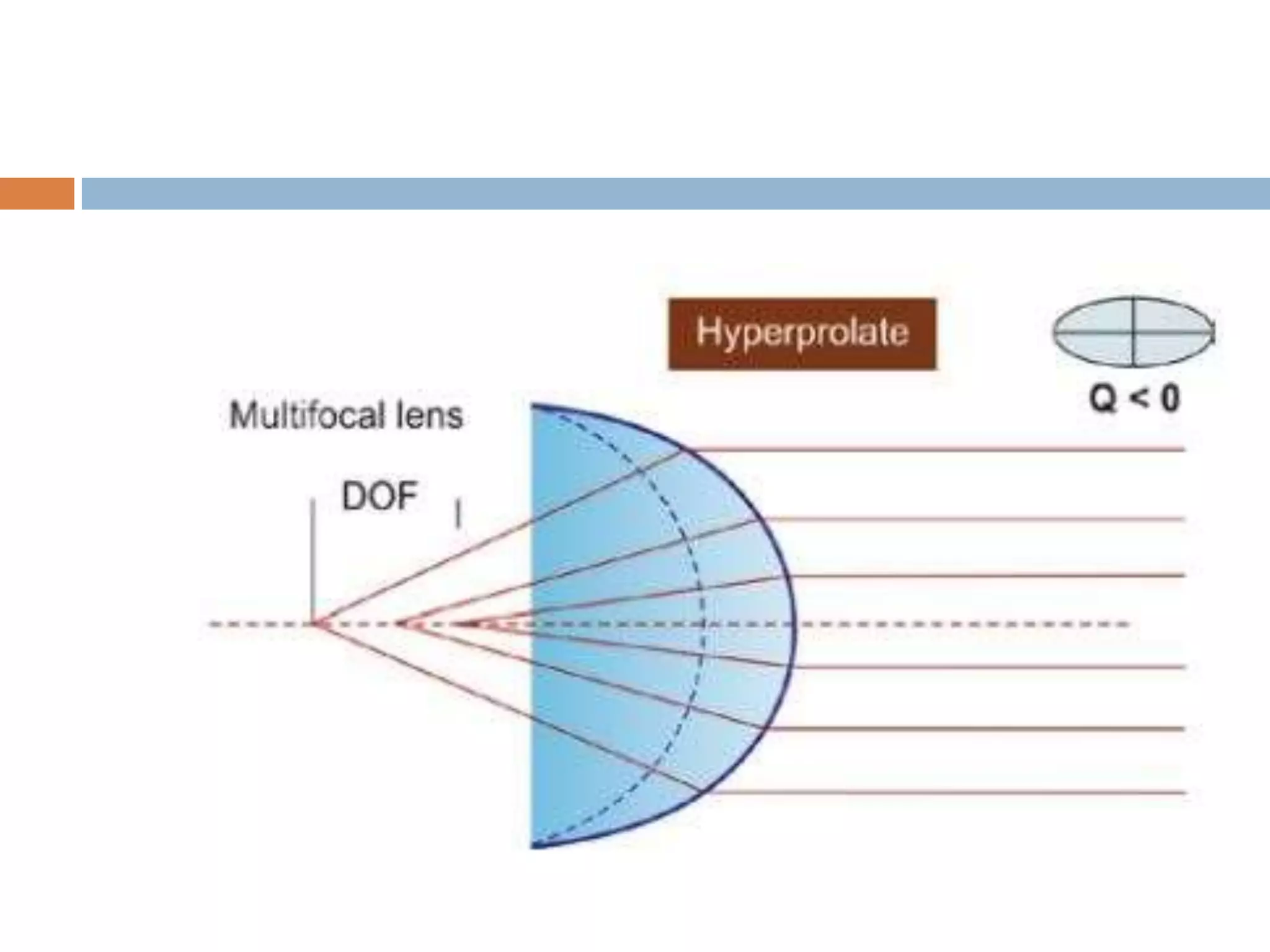
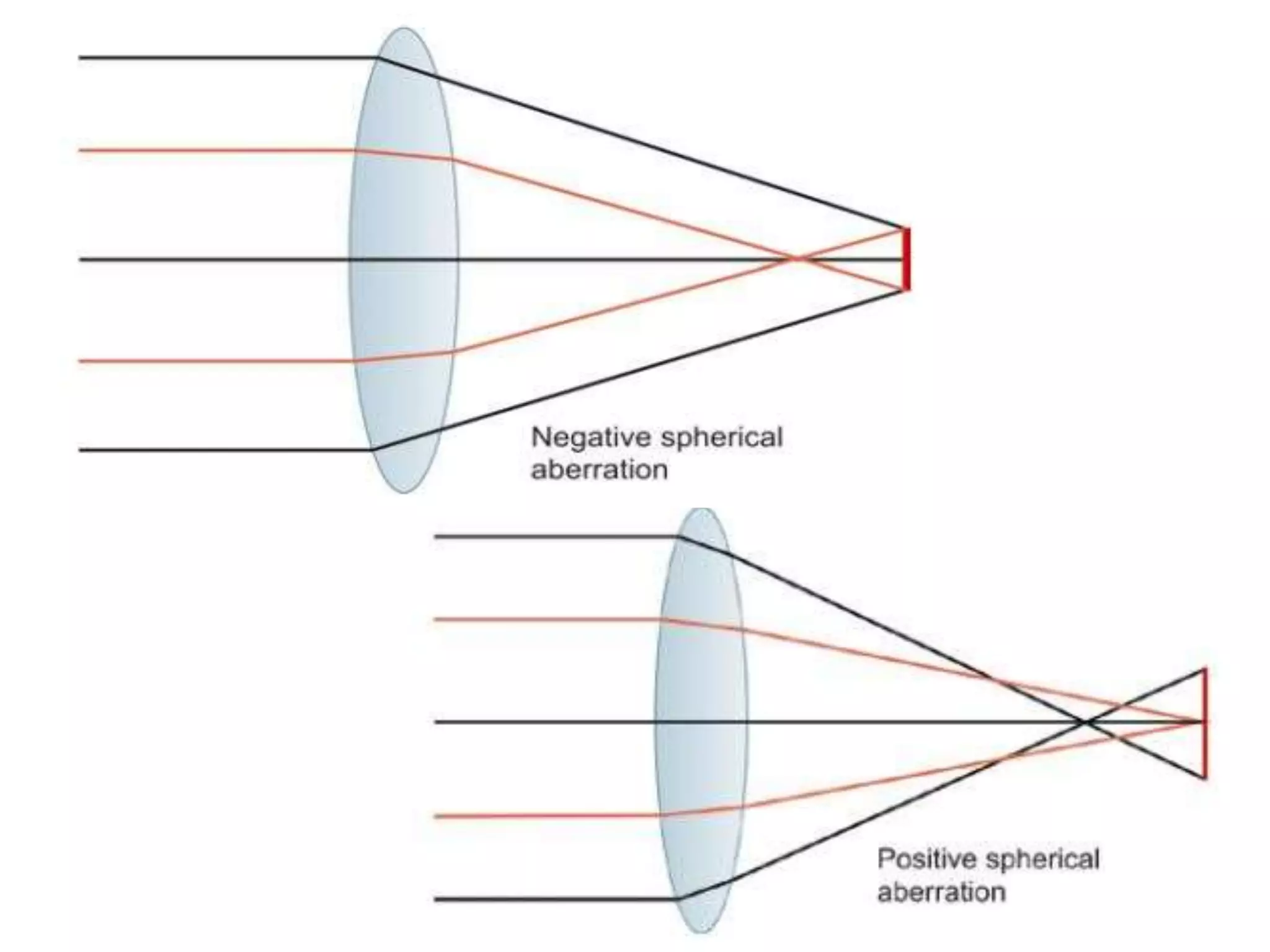
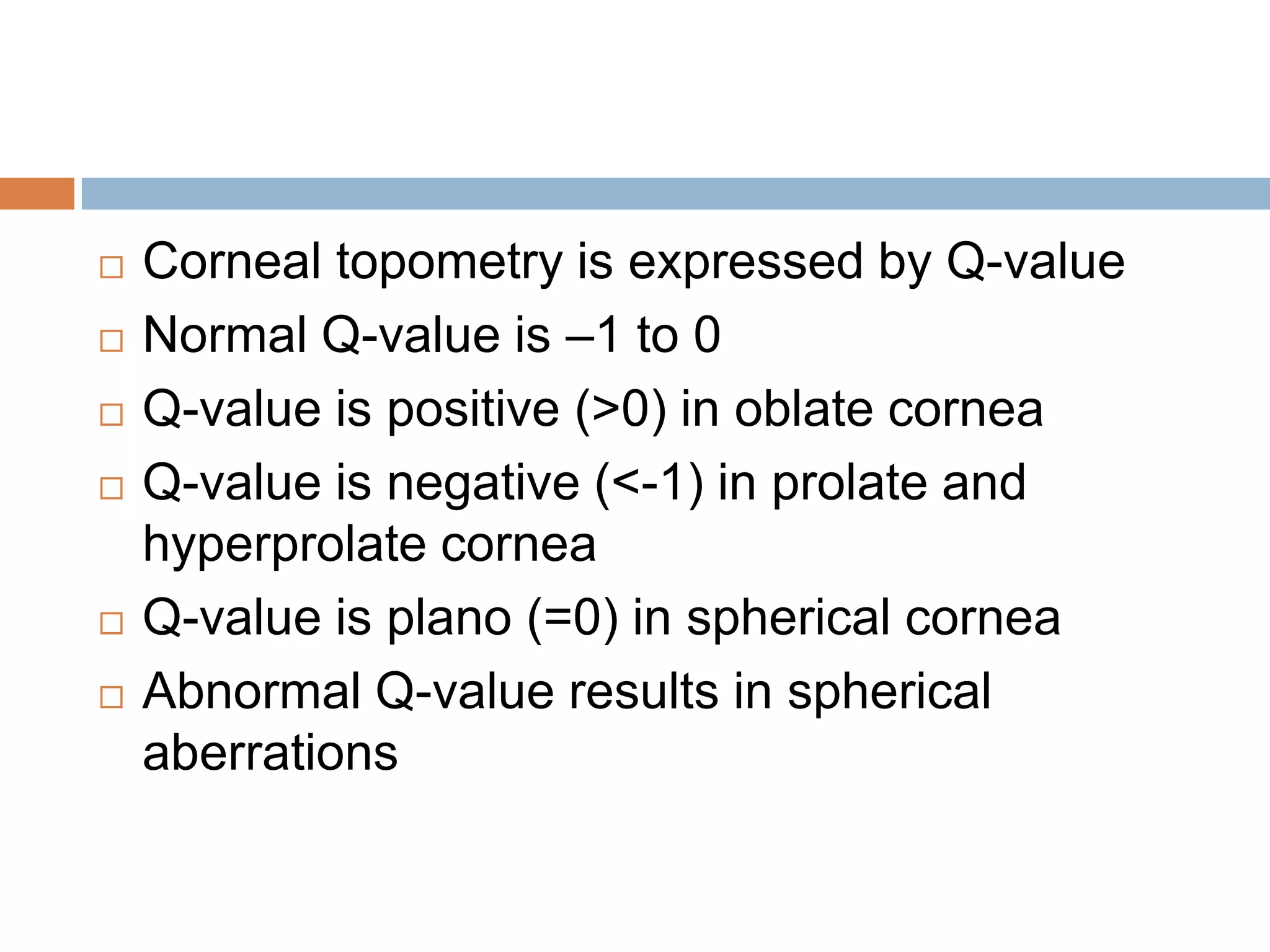
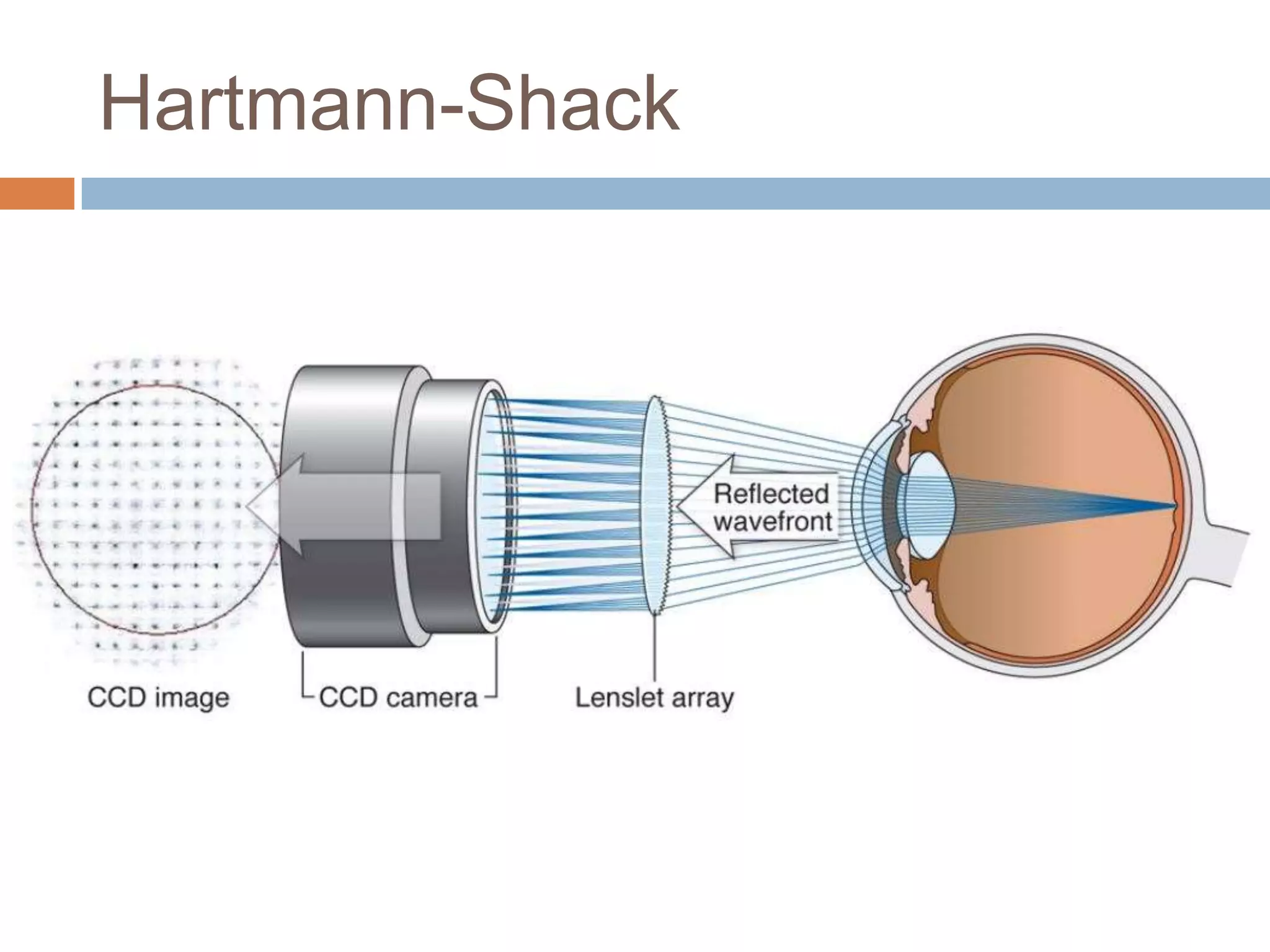
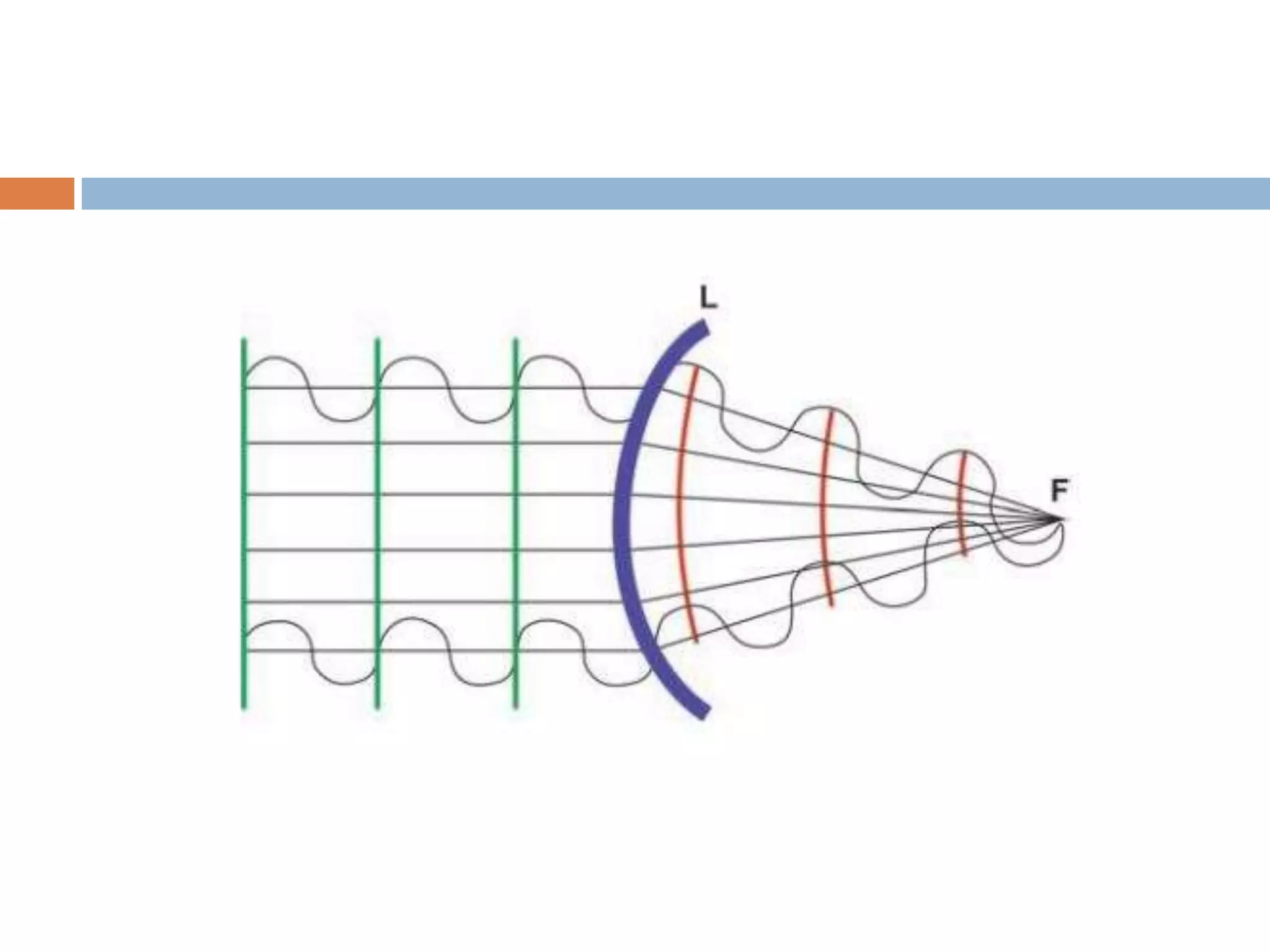
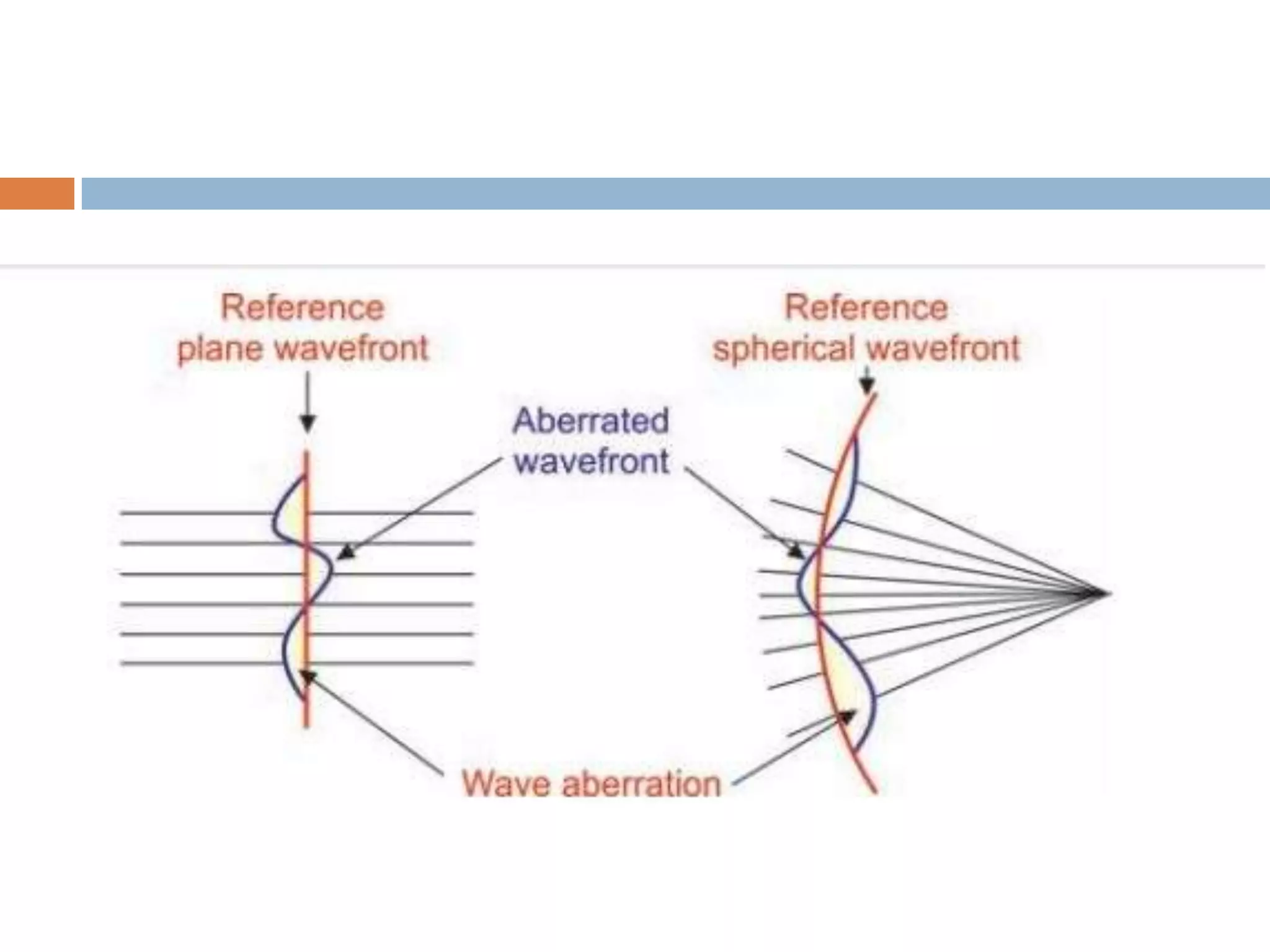
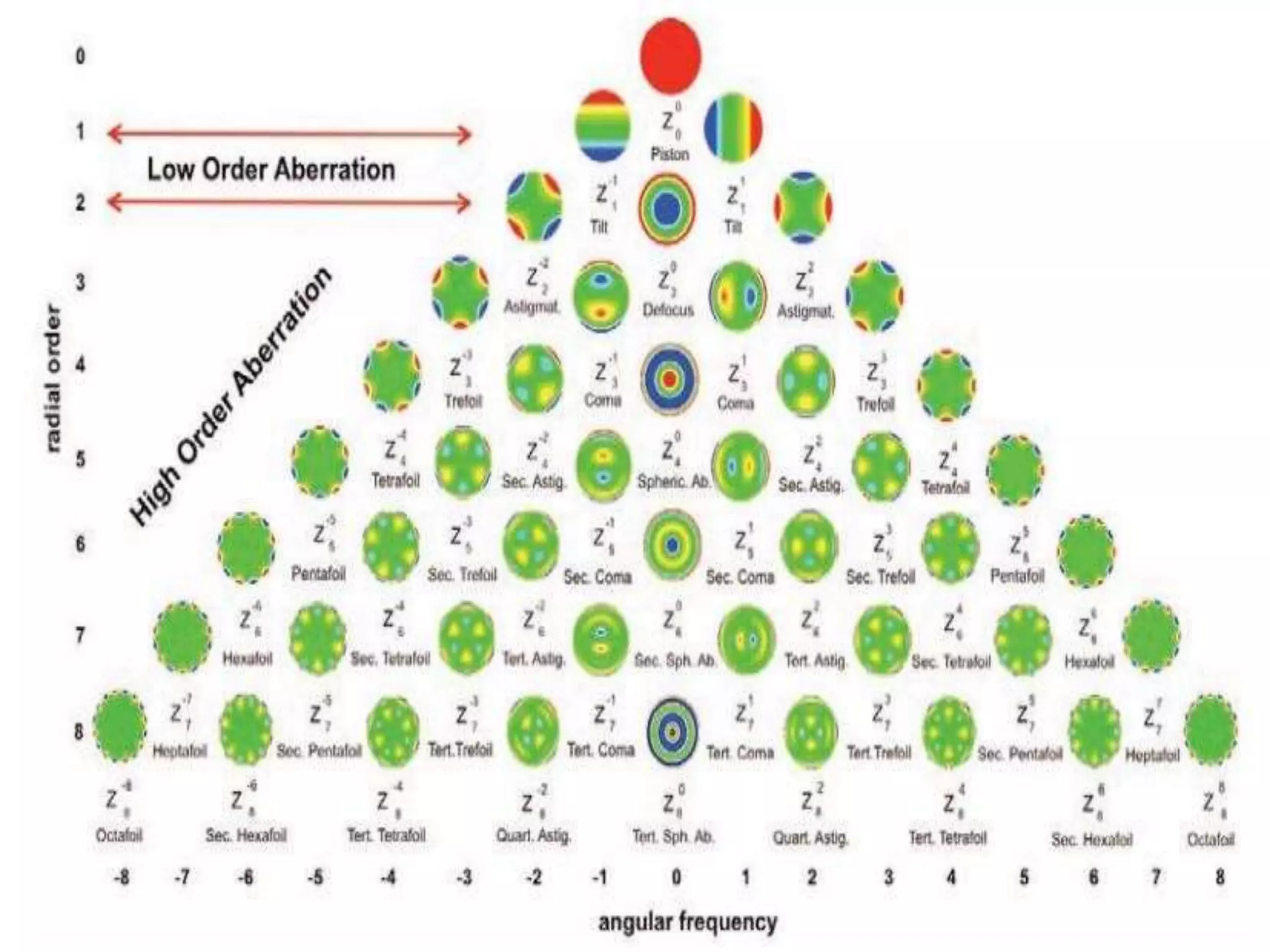
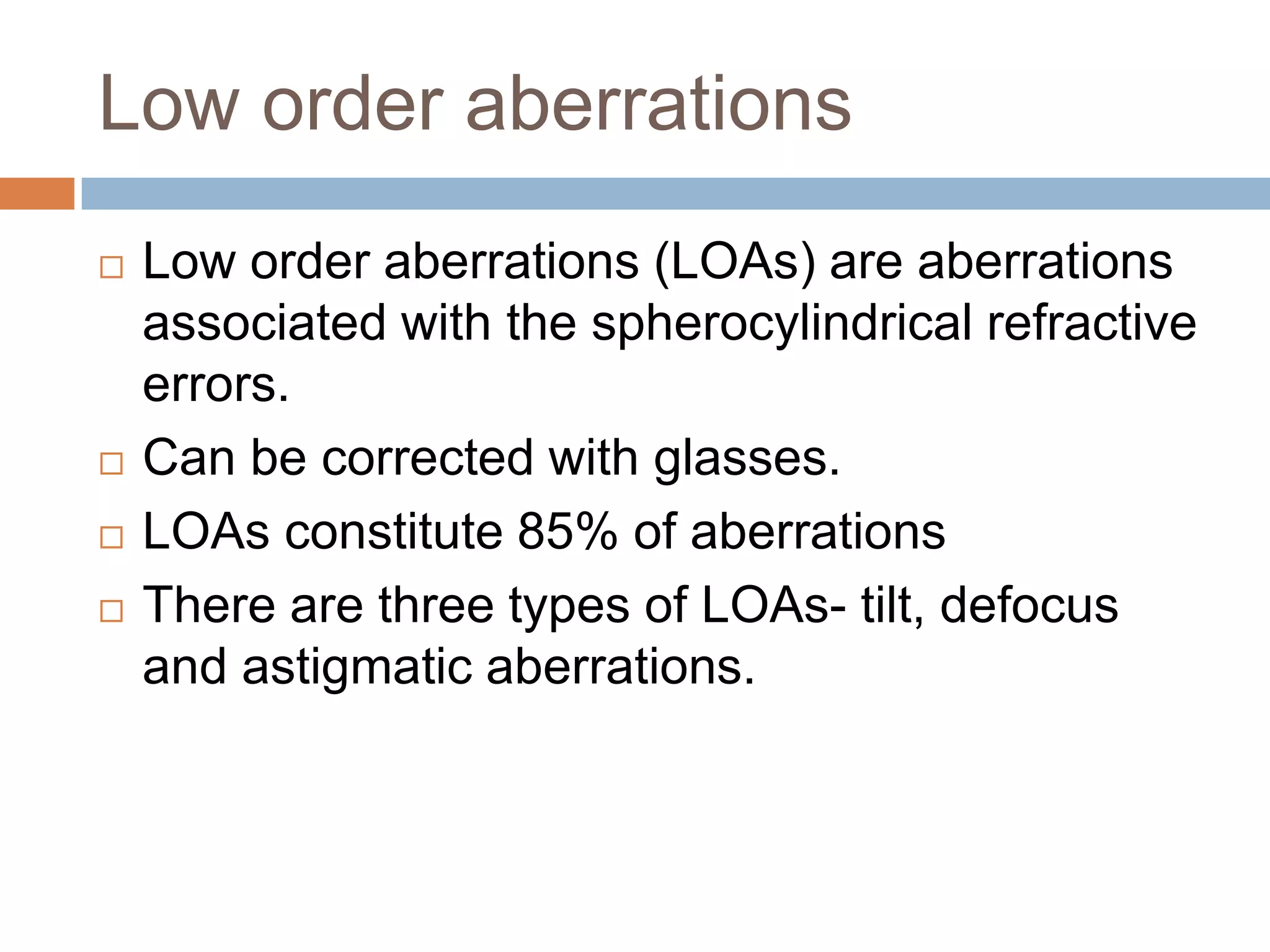
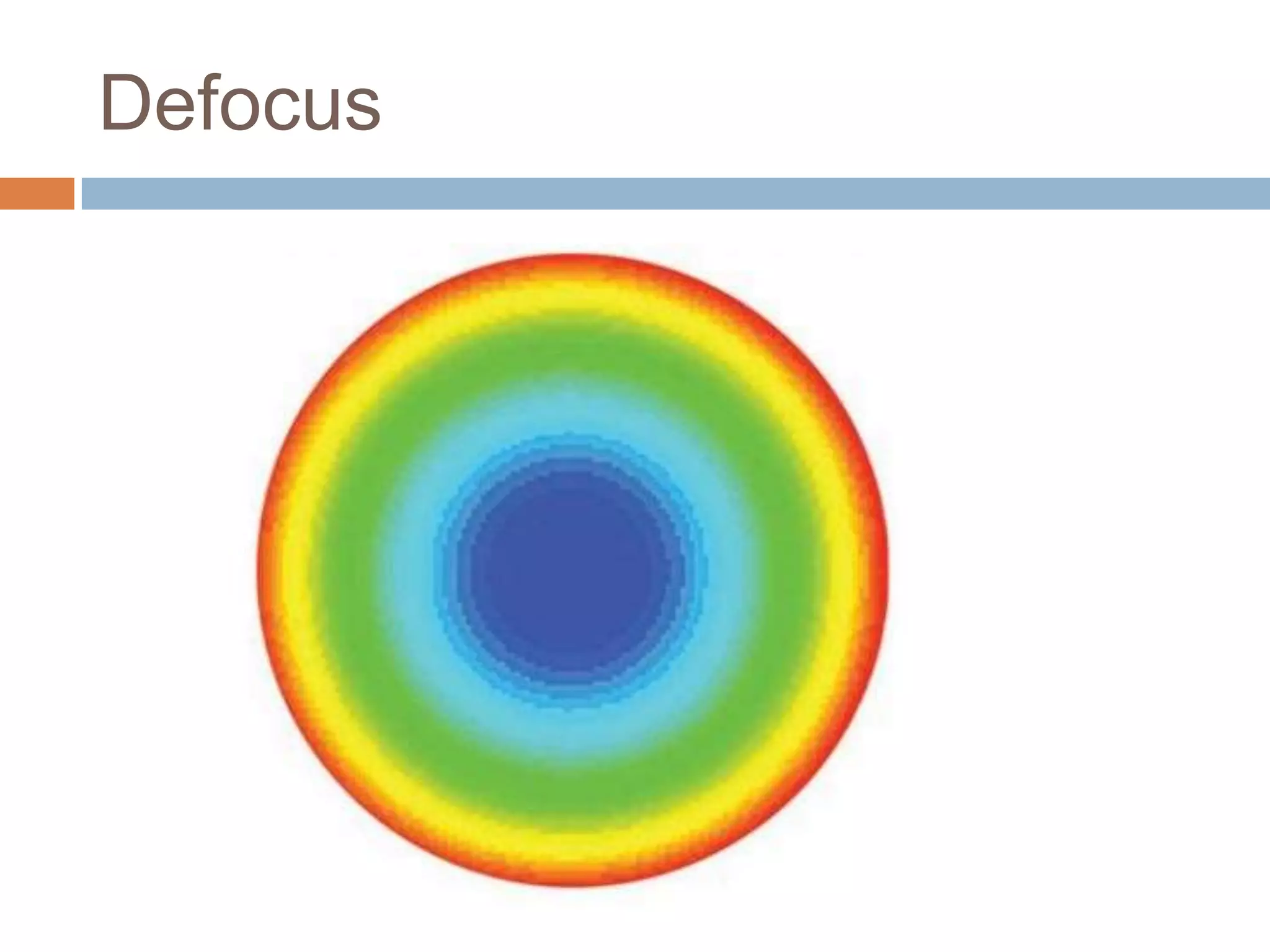
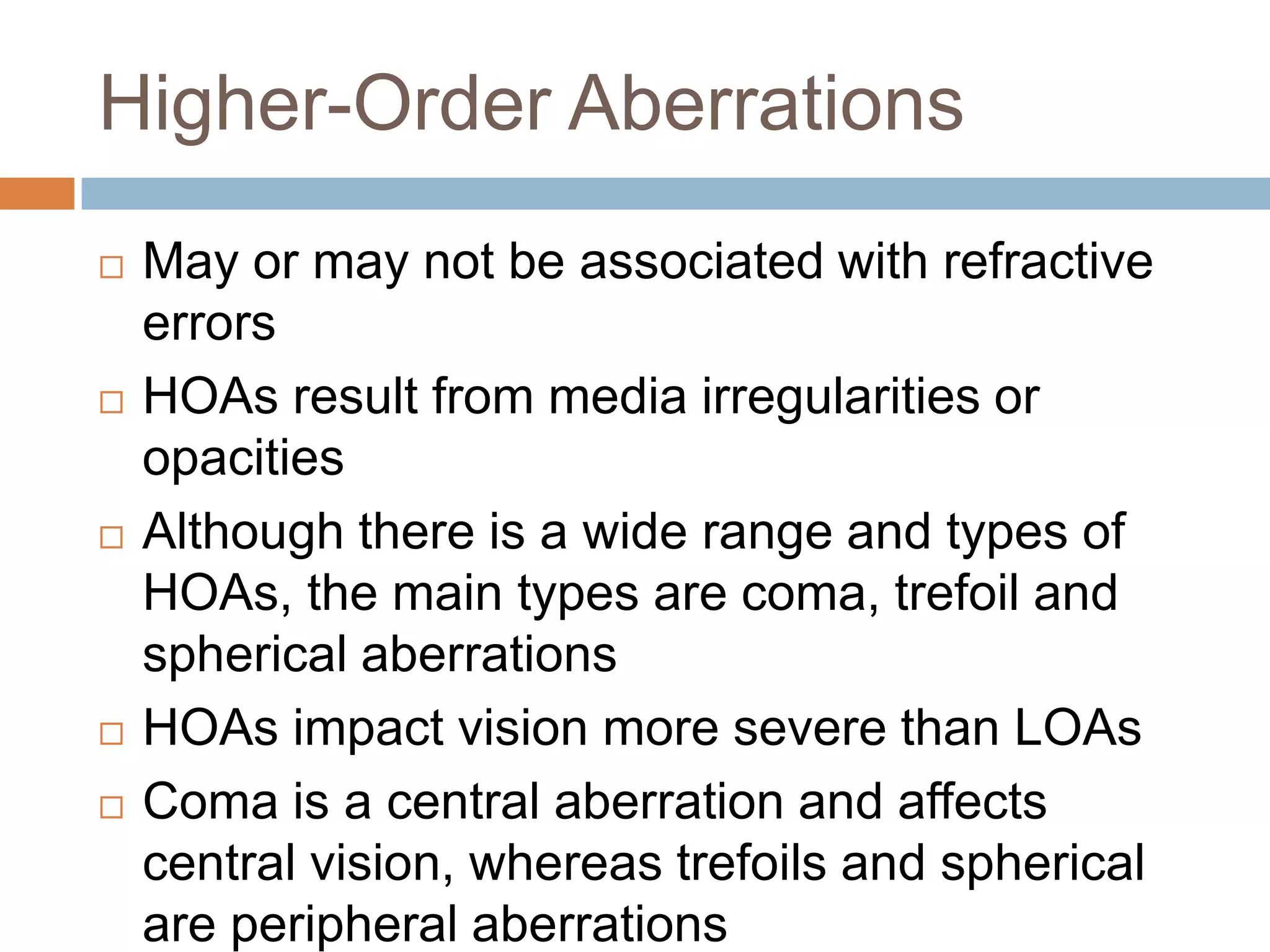
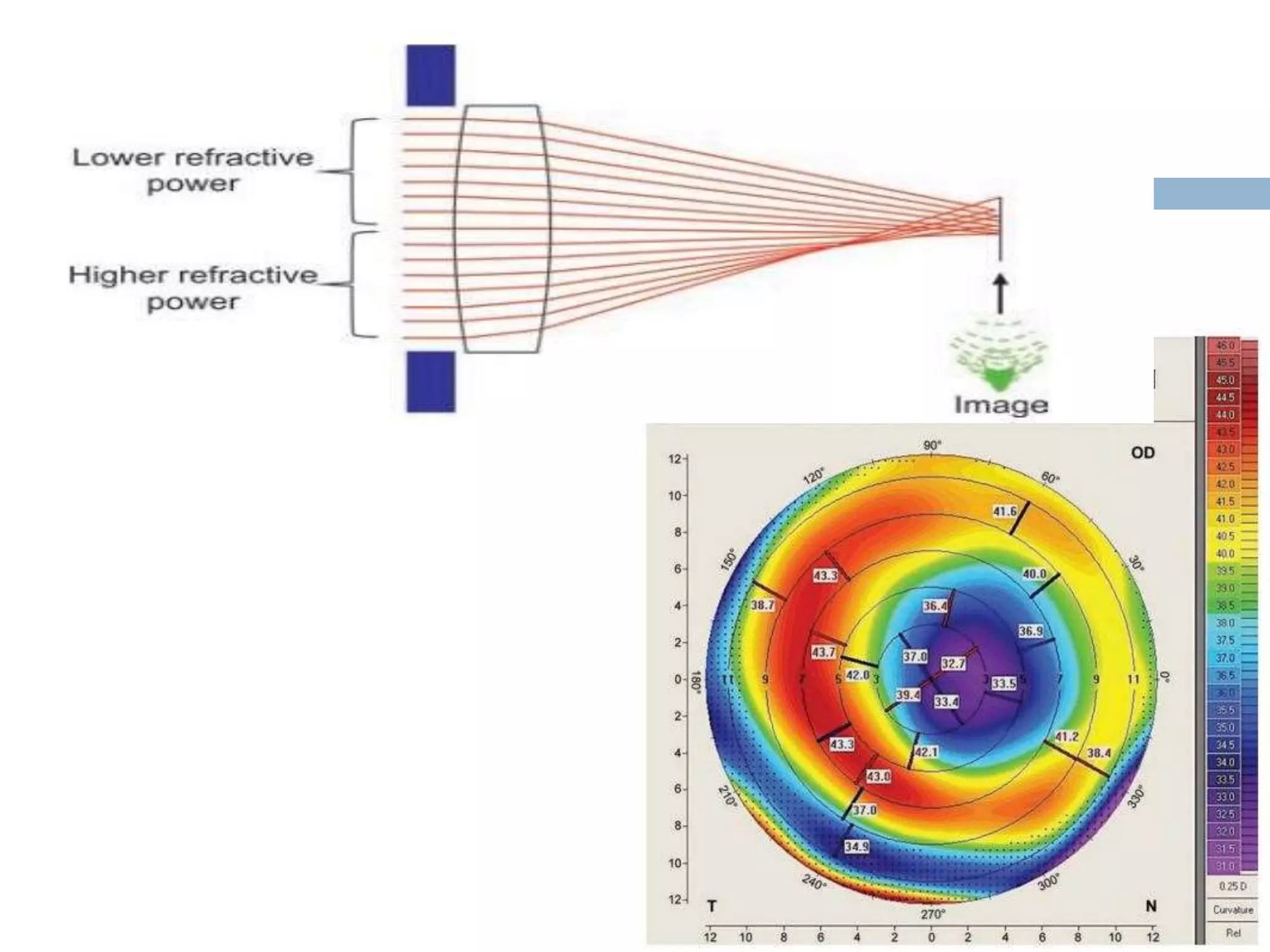
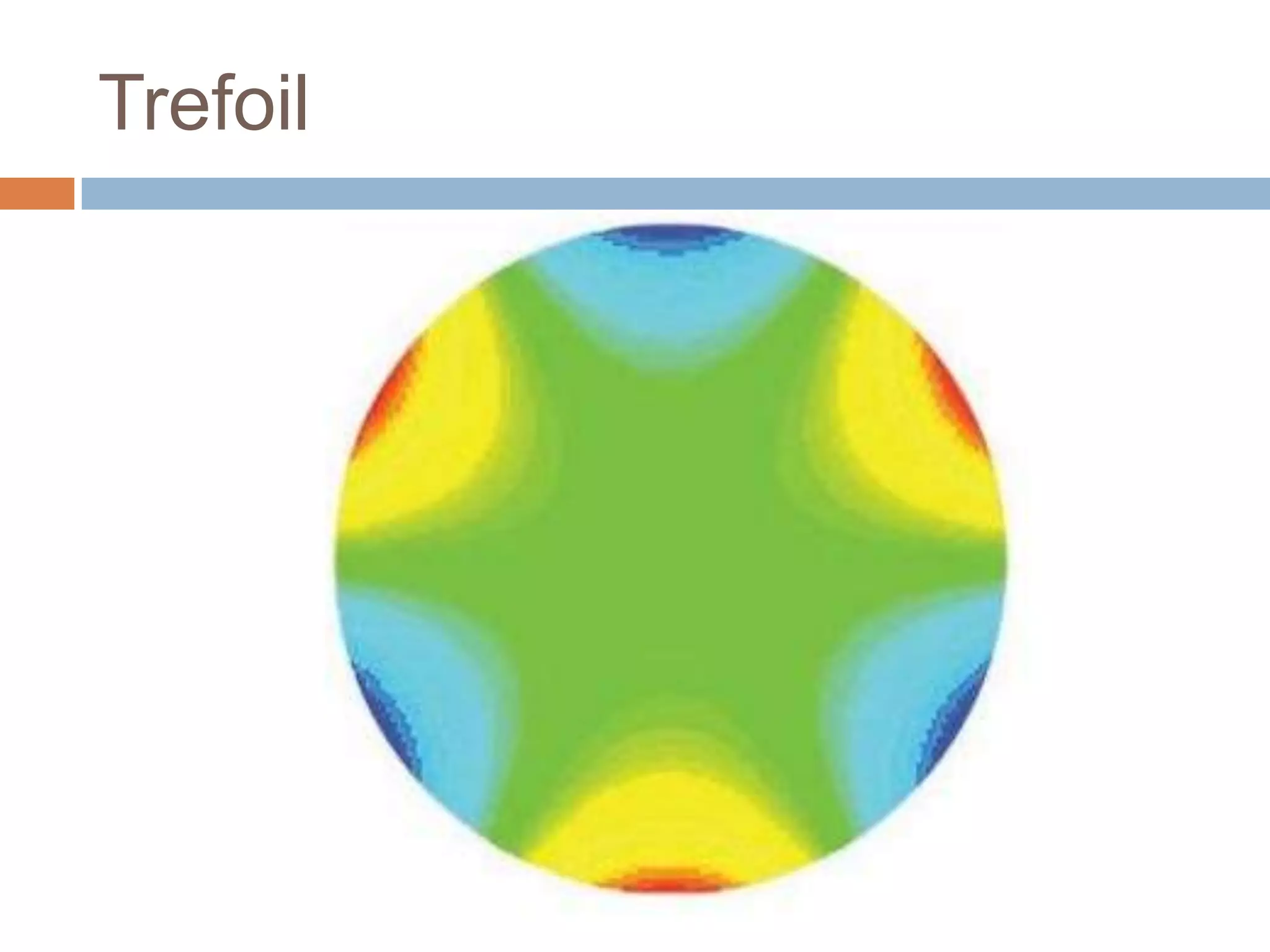
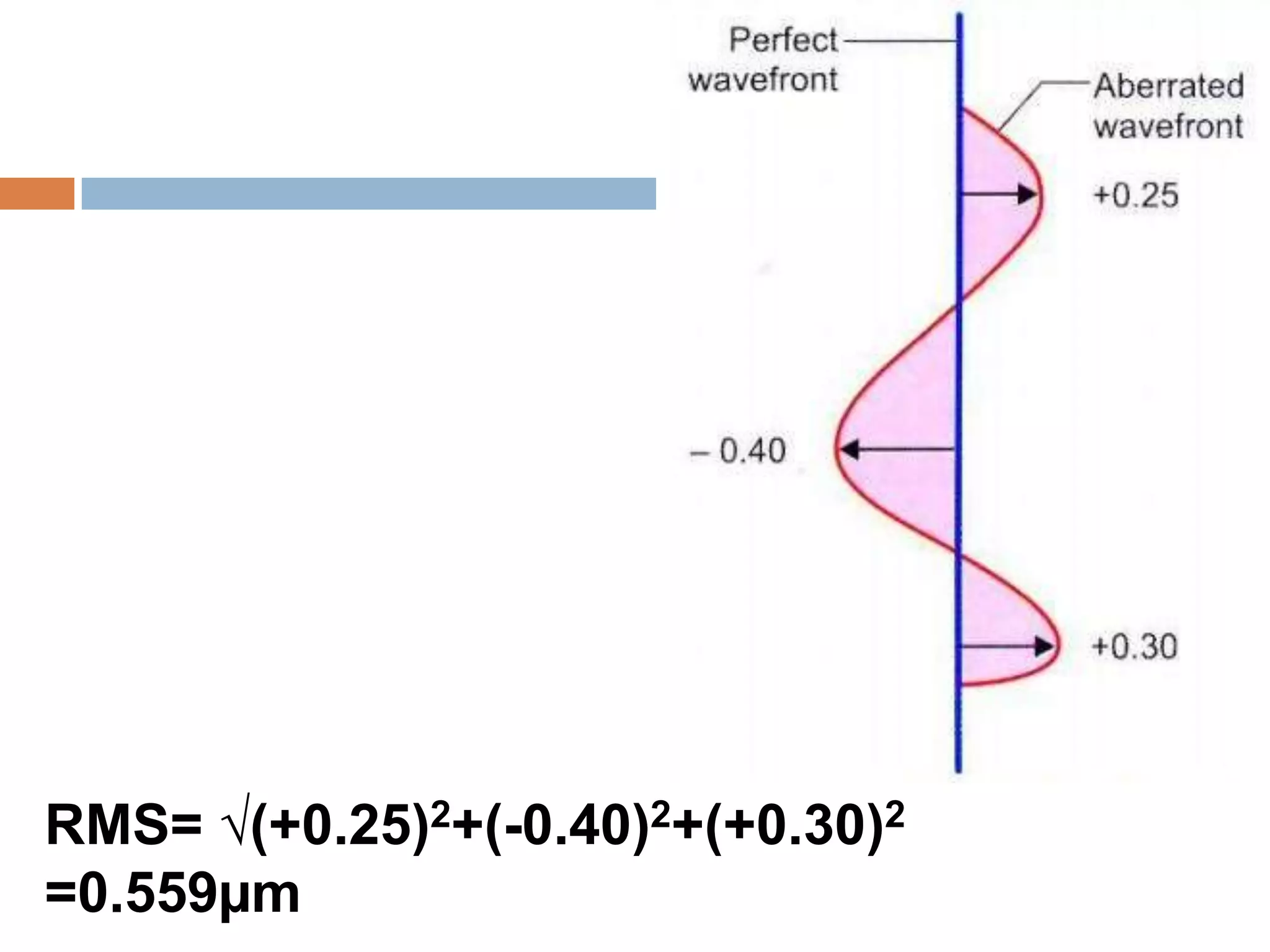
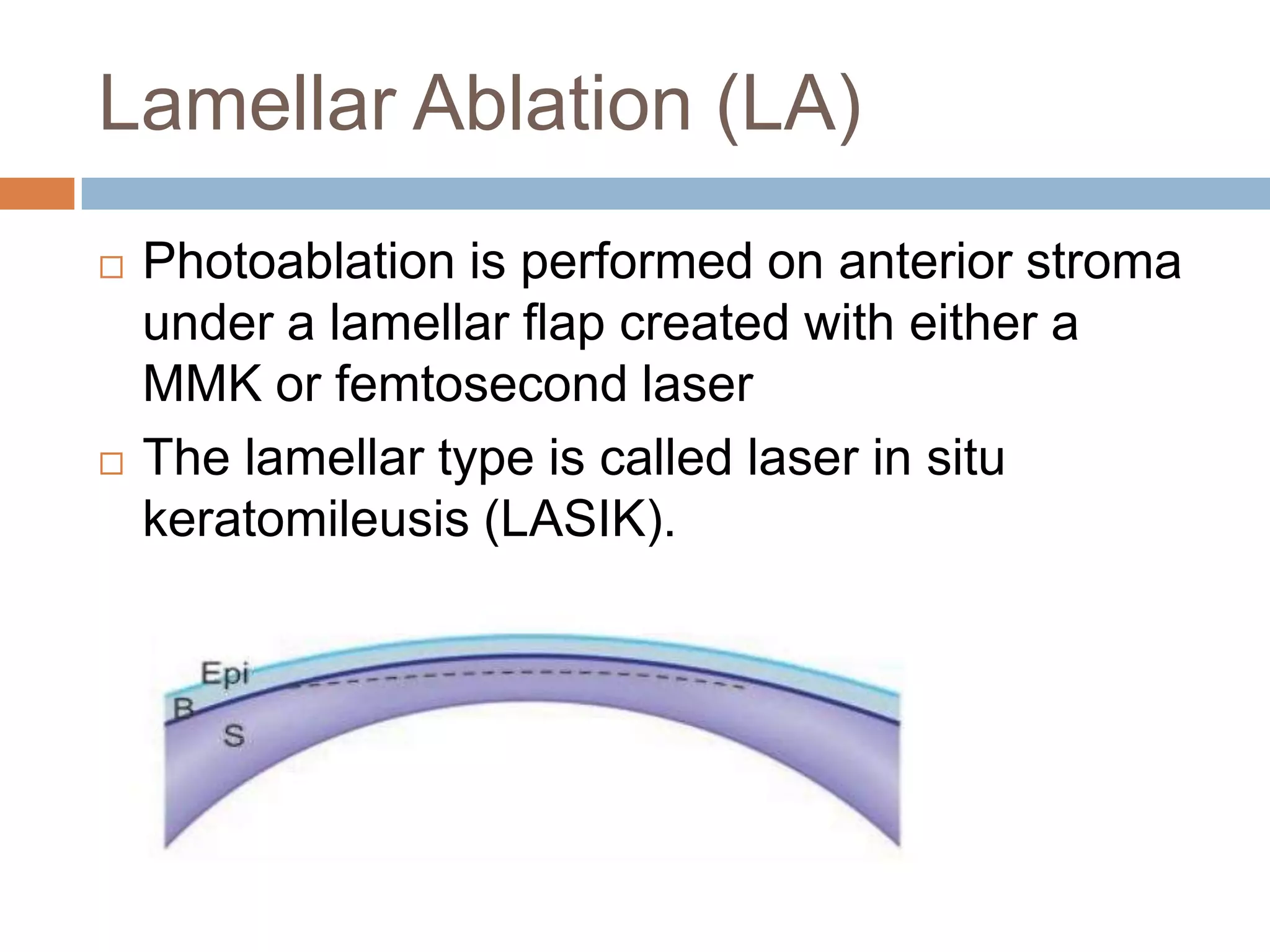
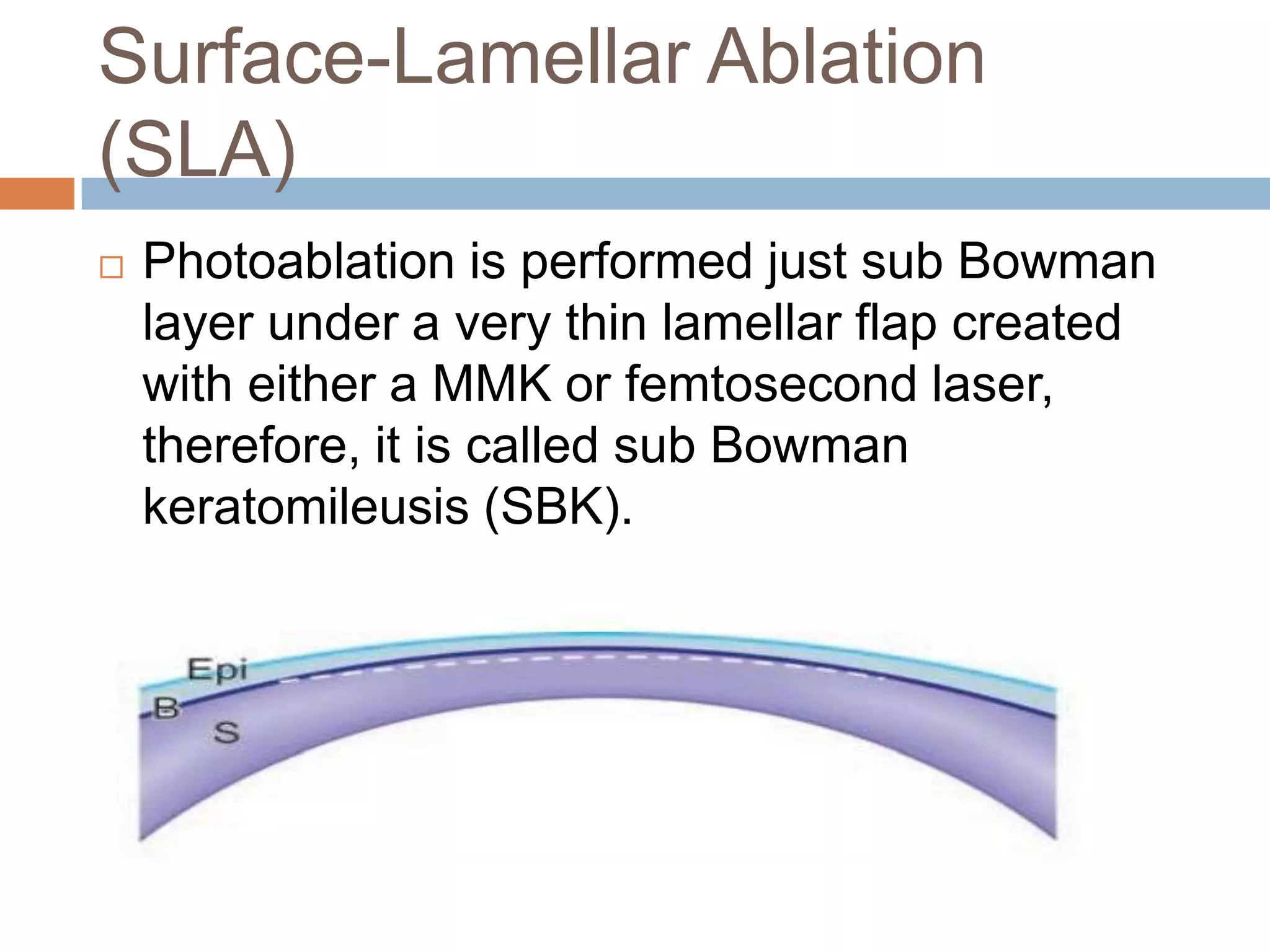
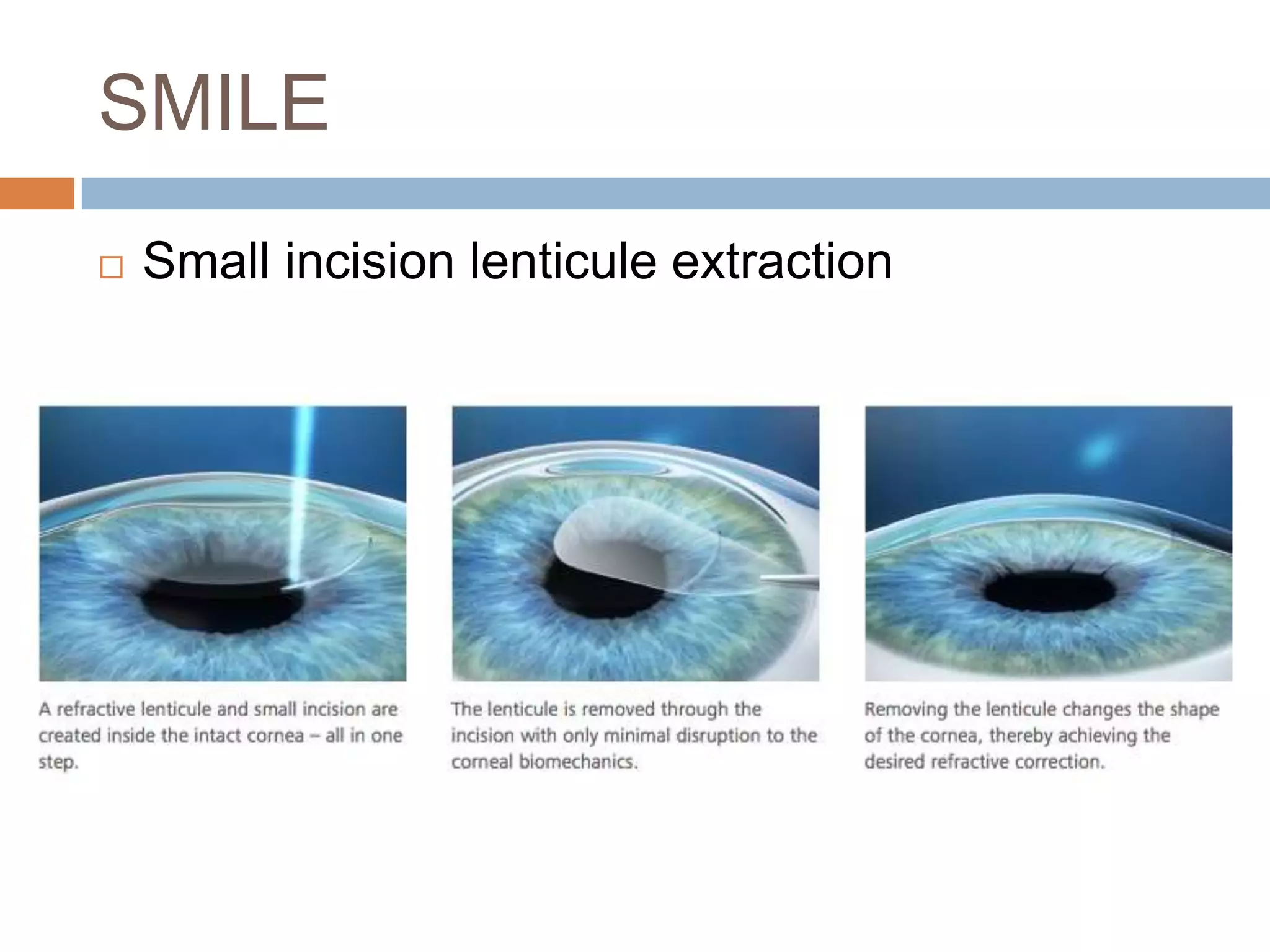
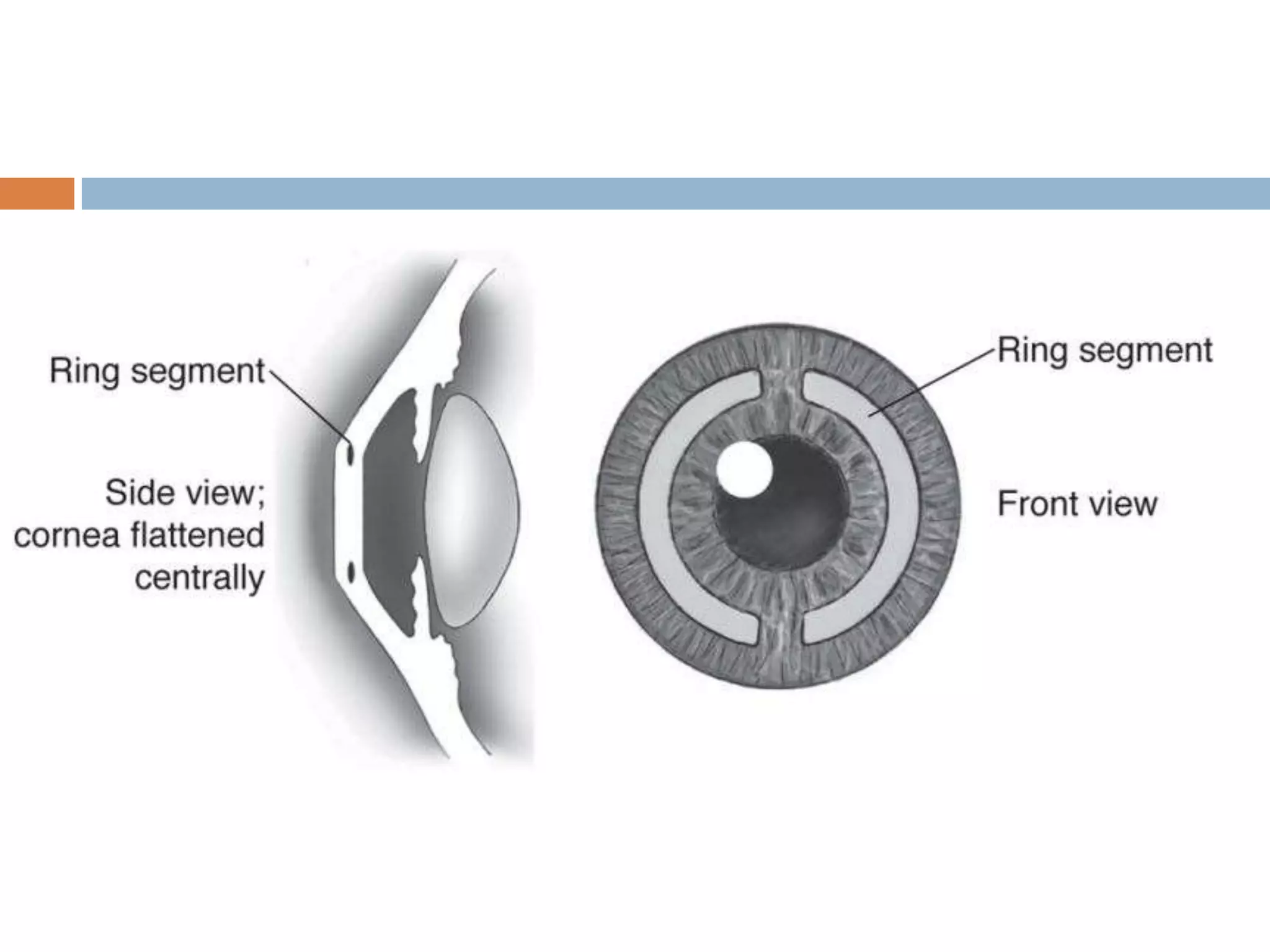
The document discusses various aspects of patient evaluation and treatment options for refractive surgery. It describes evaluating a patient's psychosocial factors, medical and ocular history, and examination findings to determine suitability for different refractive surgery techniques. A variety of surgical options are outlined including corneal procedures like LASIK, PRK, and lens-based procedures. Topics like wavefront analysis and assessing higher-order aberrations are also summarized.