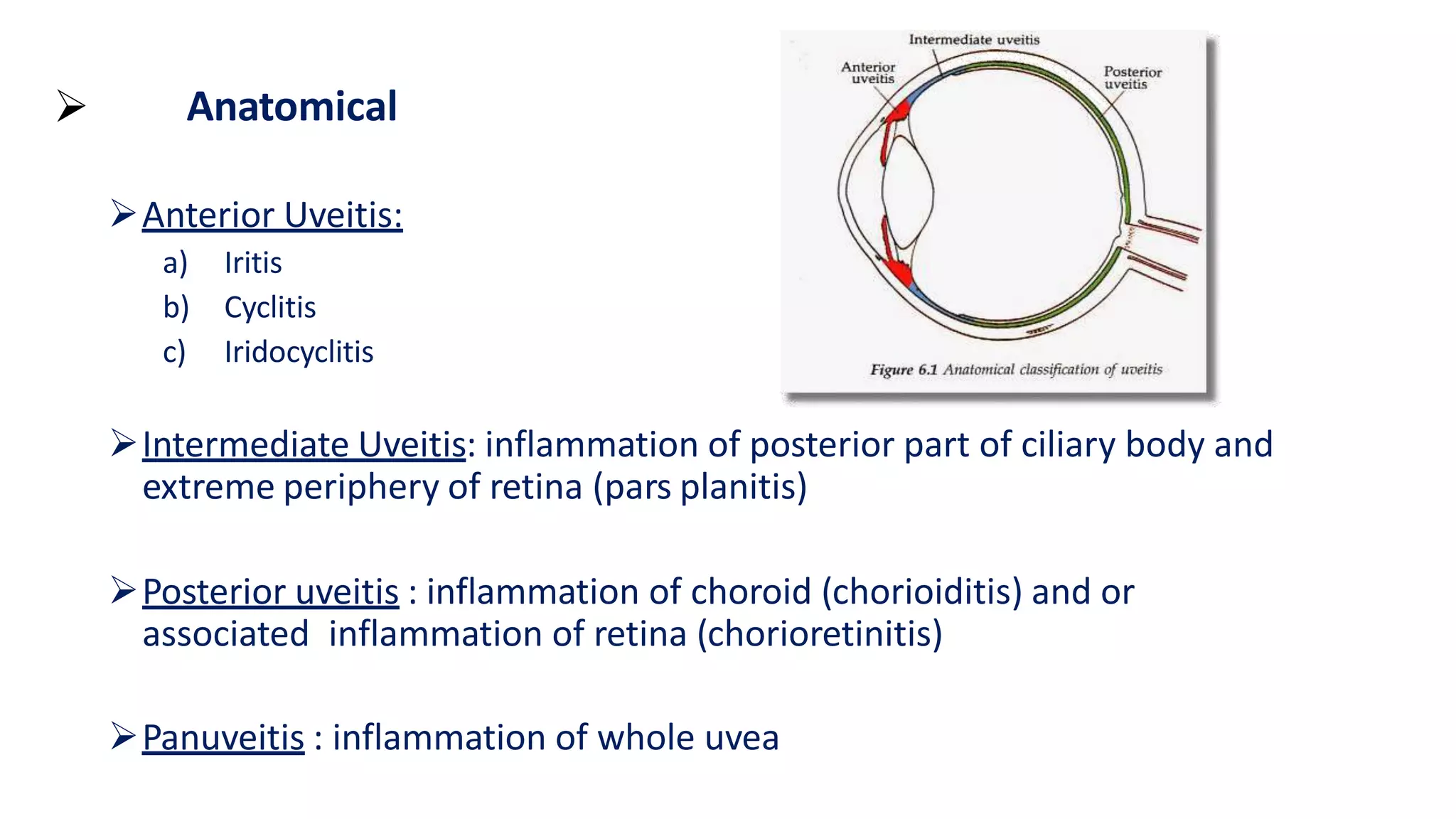
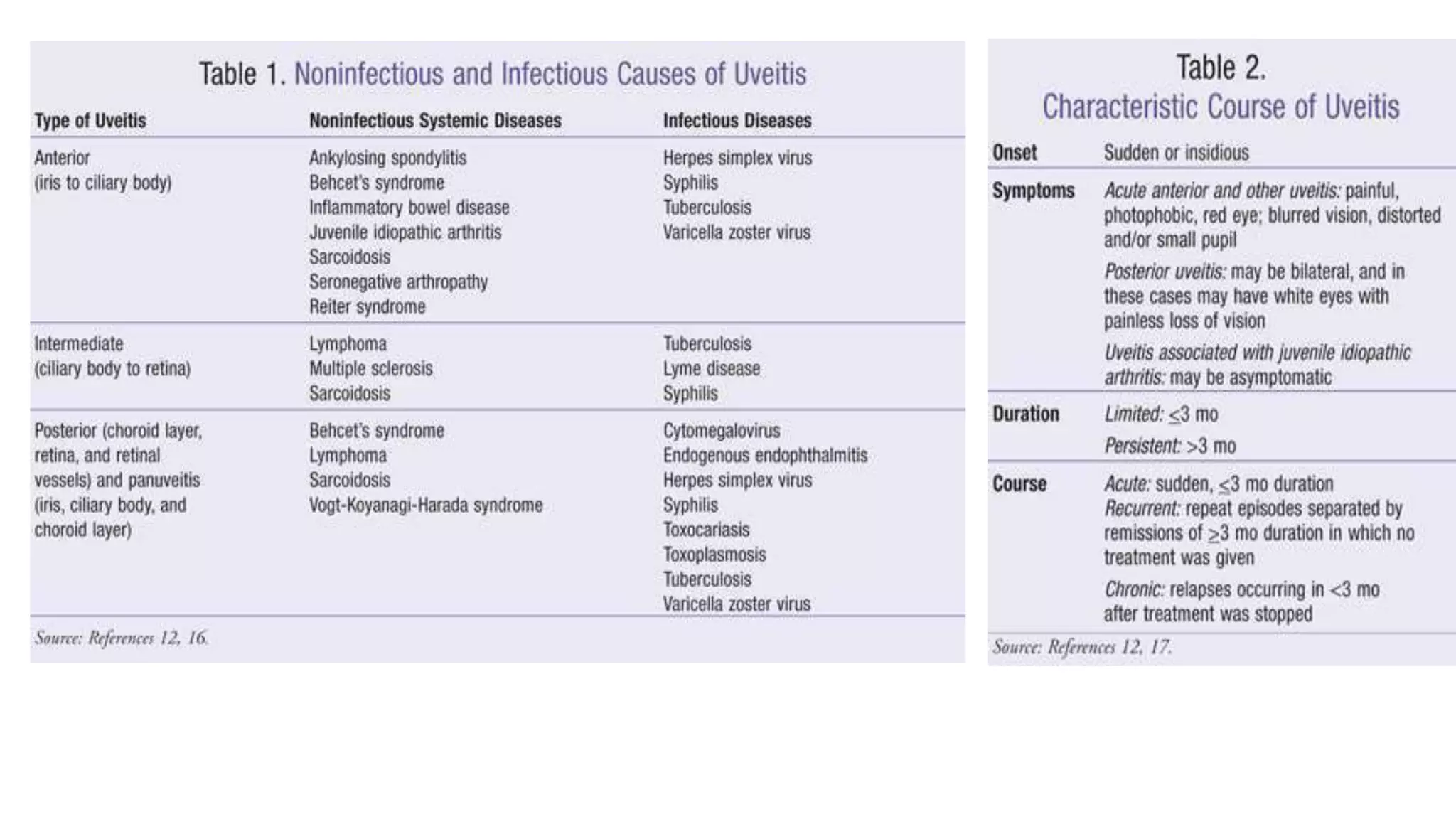
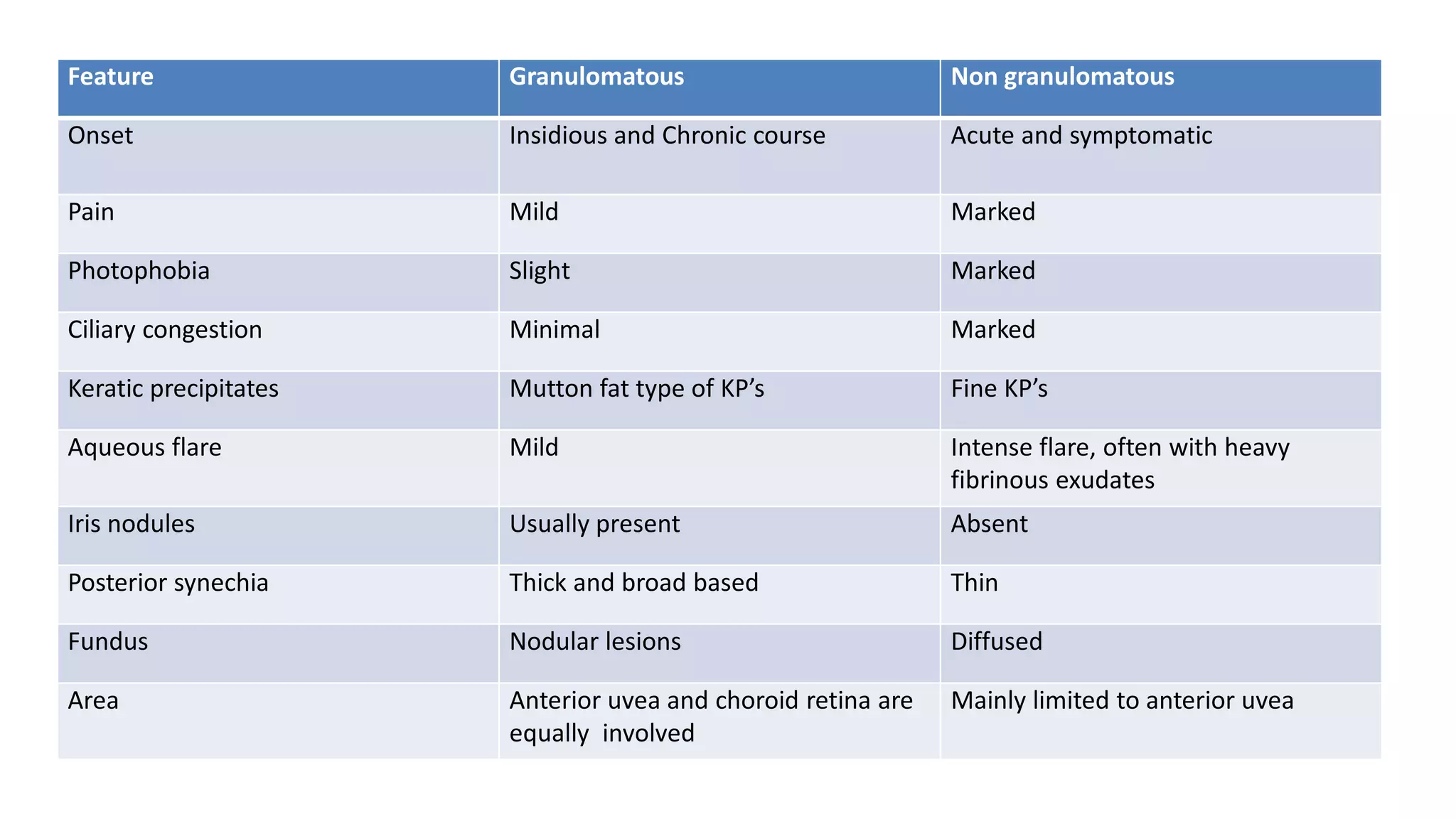
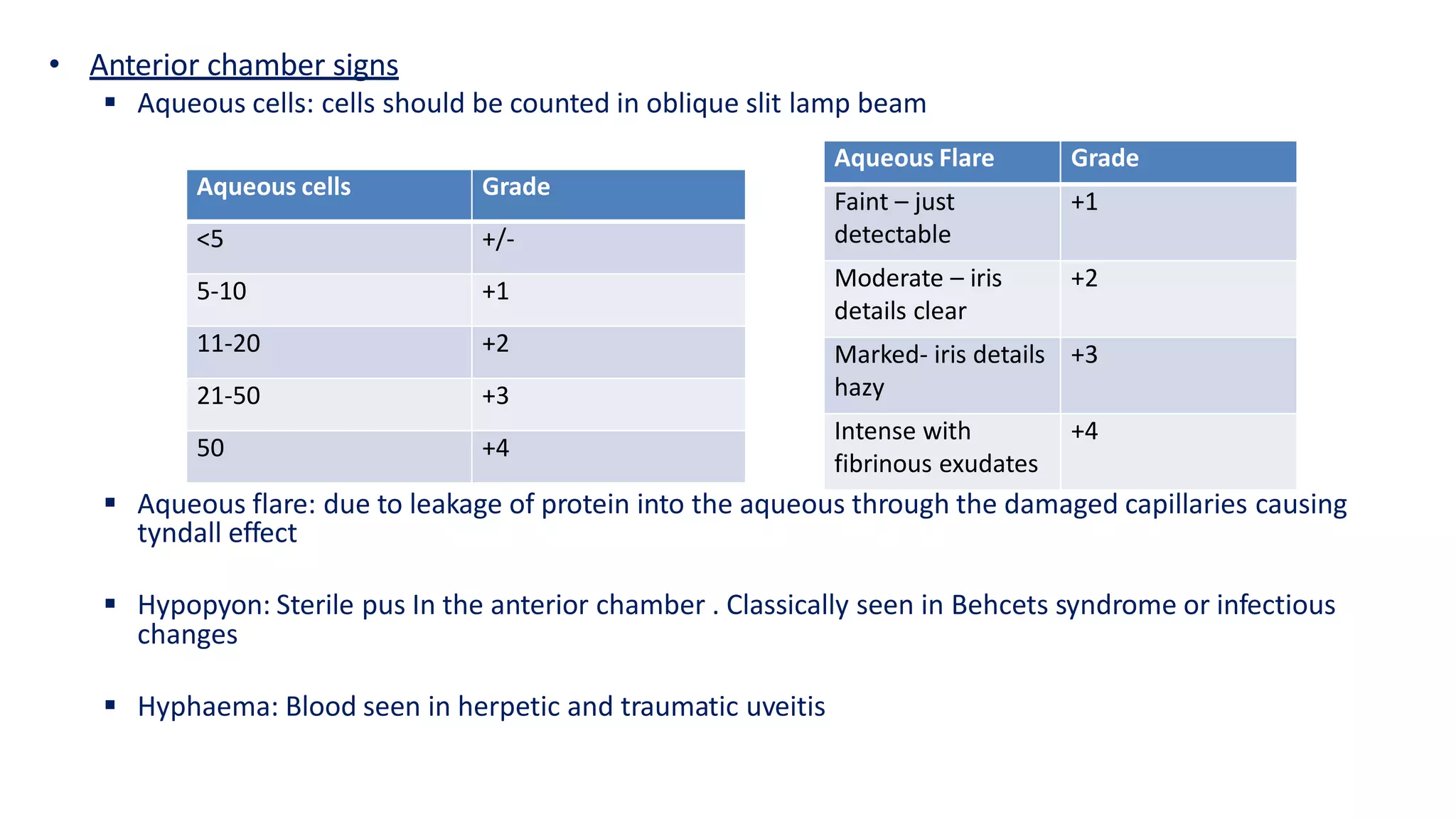
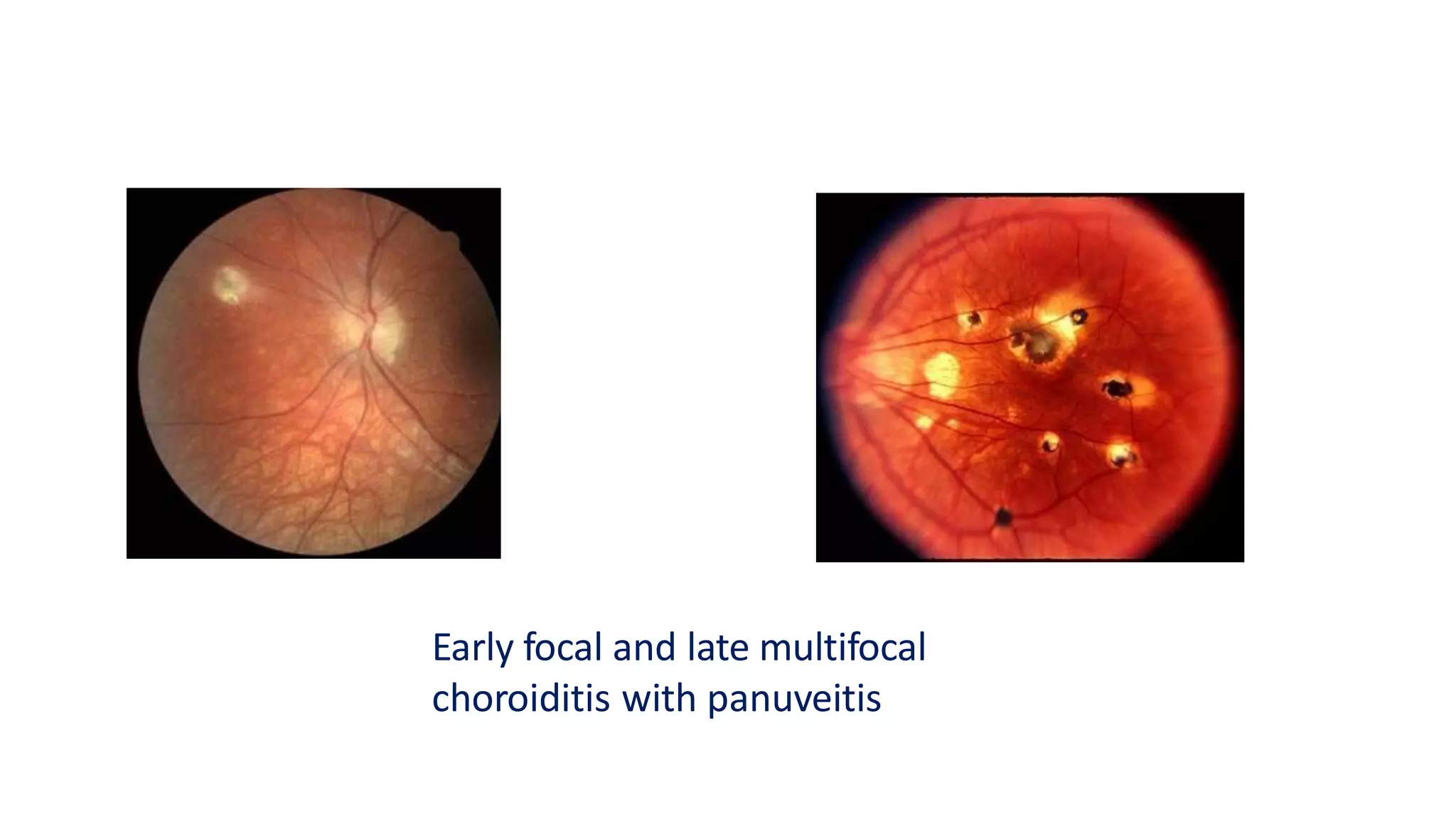
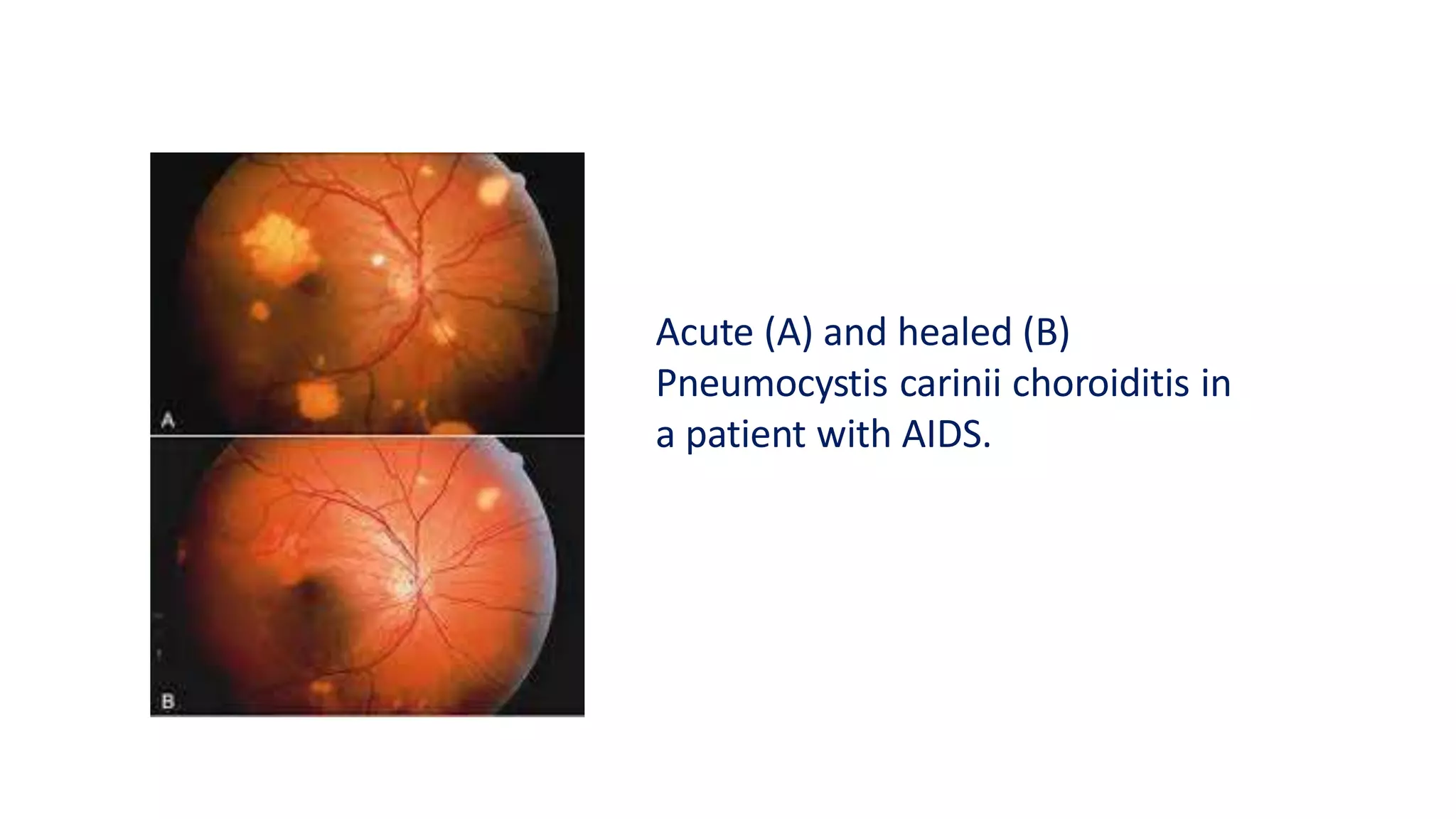
This document discusses uveitis, which is inflammation of the uveal tract of the eye. It is classified anatomically by the area of inflammation (anterior, intermediate, posterior), clinically by duration (acute or chronic), pathologically by inflammatory cell type (granulomatous or non-granulomatous), and etiologically by cause. Anterior uveitis causes pain, redness and photophobia, and signs include cells in the aqueous humor and keratic precipitates on the cornea. Posterior uveitis involves the choroid and retina, causing blurred vision and floaters, with signs of vitreous inflammation and chorioretinal lesions. Treatment involves topical or systemic cortic