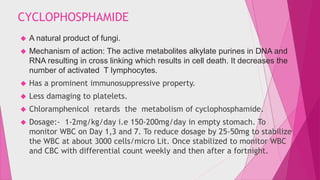
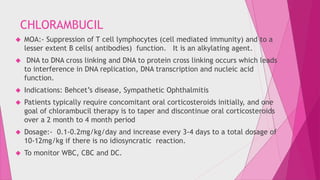
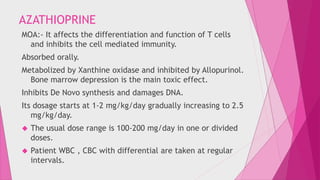
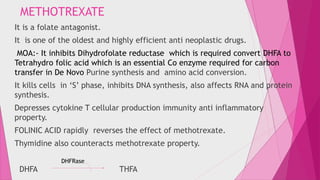
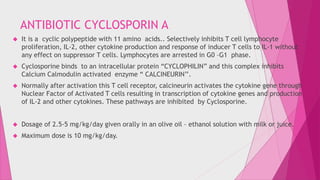
This document discusses various immunosuppressive agents used in ophthalmology, including their mechanisms of action, clinical indications, dosages, and potential adverse effects. It covers alkylating agents like cyclophosphamide and chlorambucil, antimetabolites like azathioprine and methotrexate, the antibiotic cyclosporin A, and newer agents like tacrolimus, daclizumab, and infliximab. Monitoring of blood counts is important when using these drugs due to risks of bone marrow suppression, infections, and other toxicities. Careful dosage adjustment and patient follow up is needed with immunosuppressive therapy for ocular conditions.