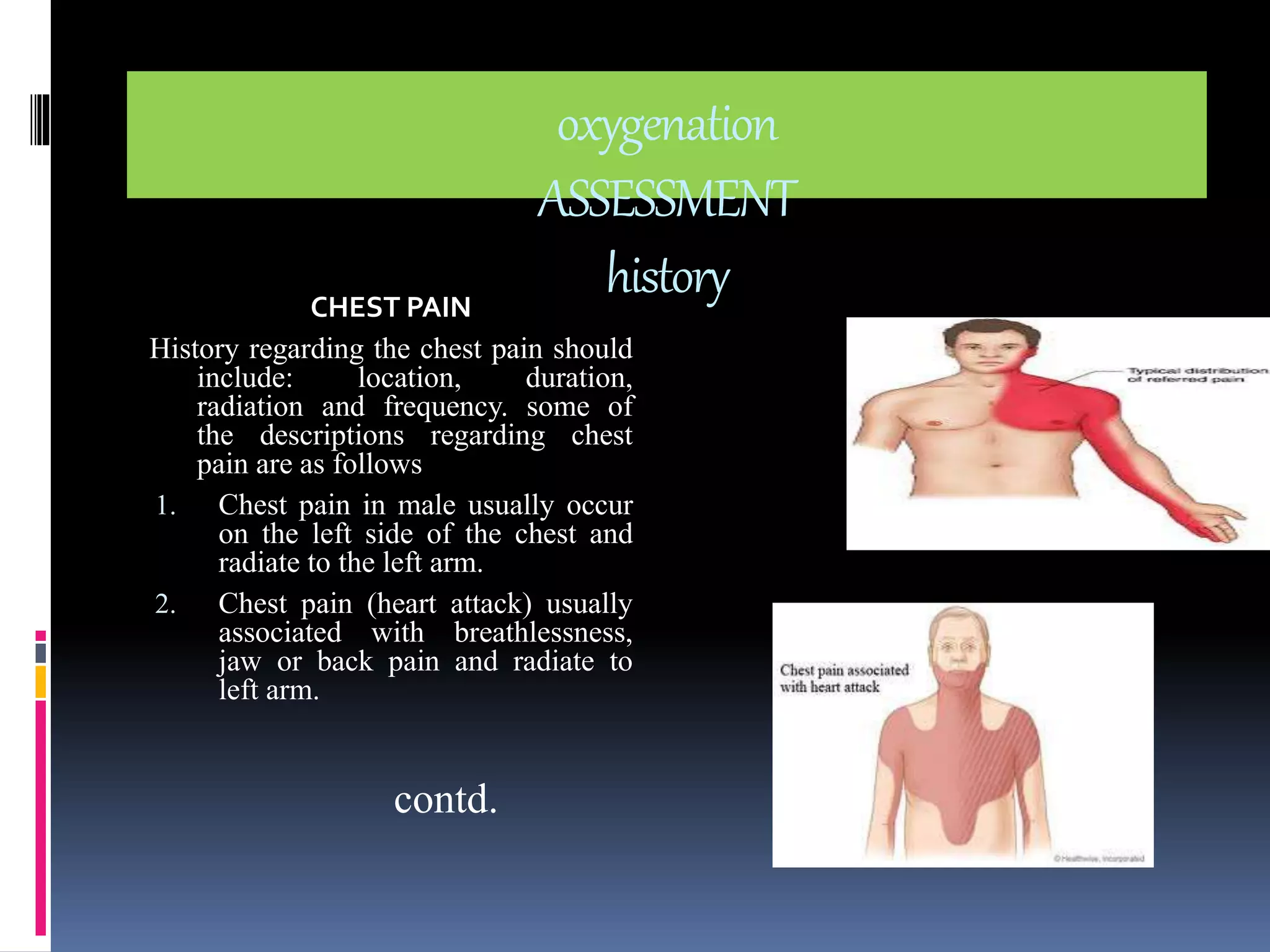
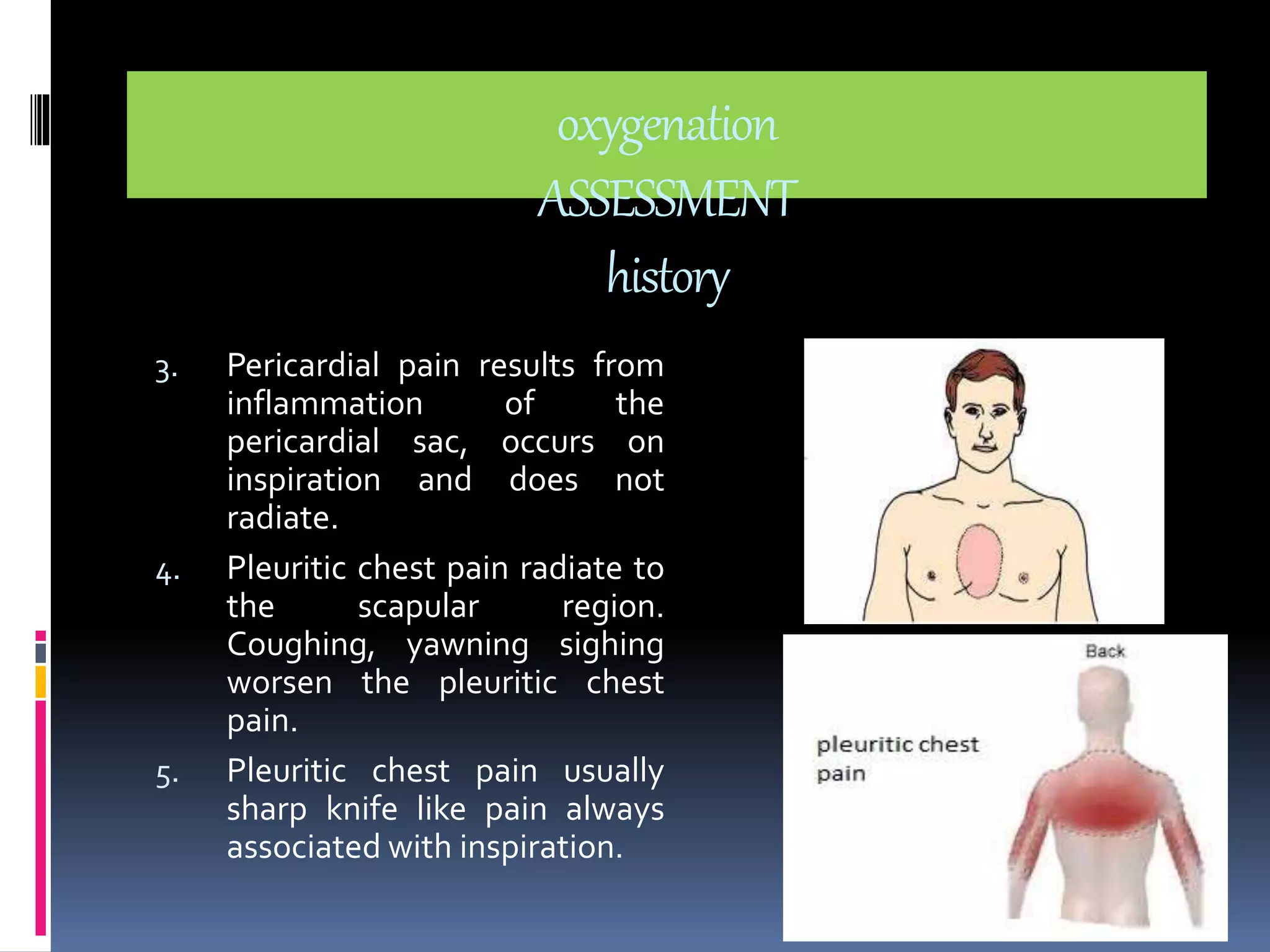
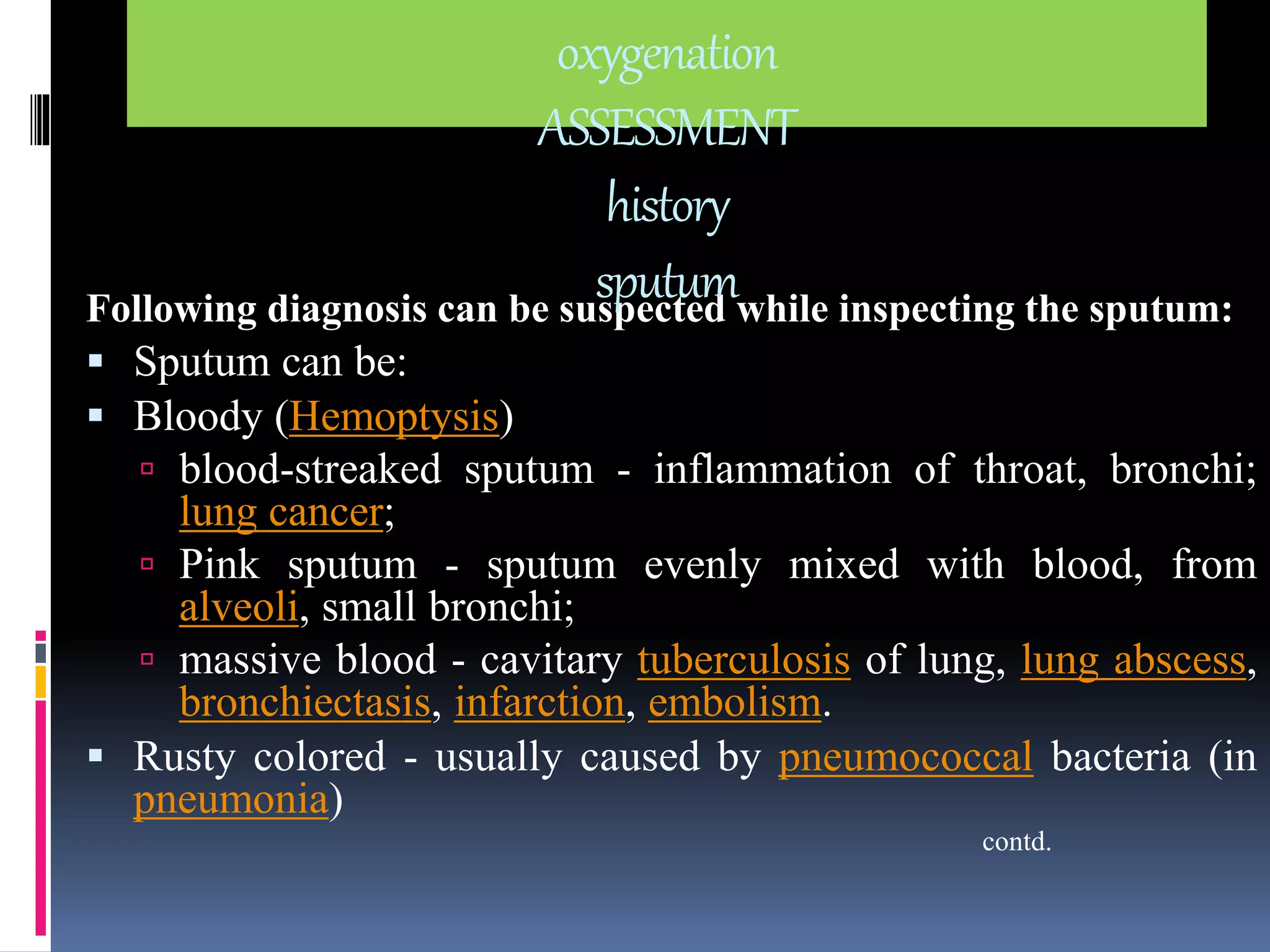
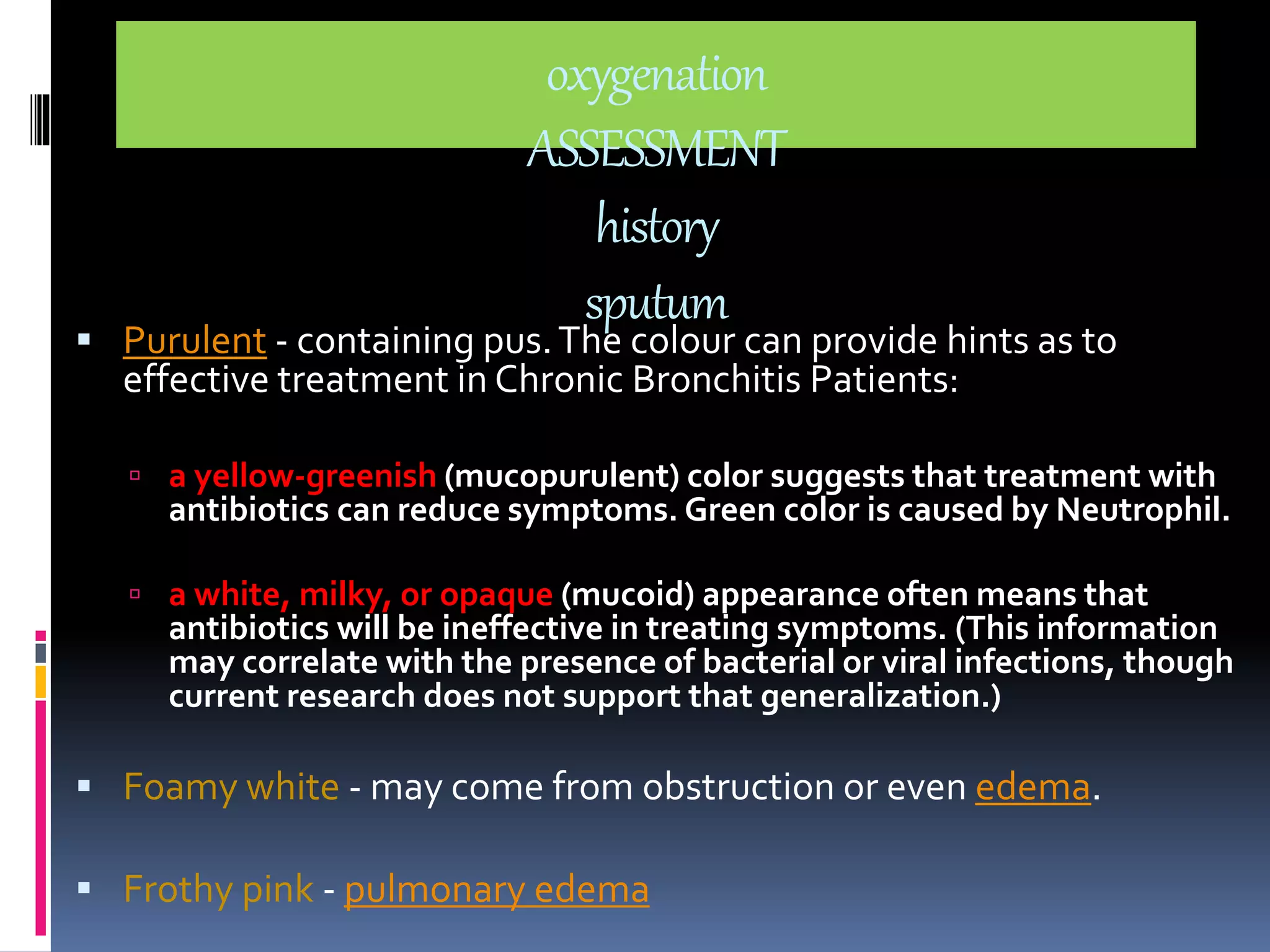
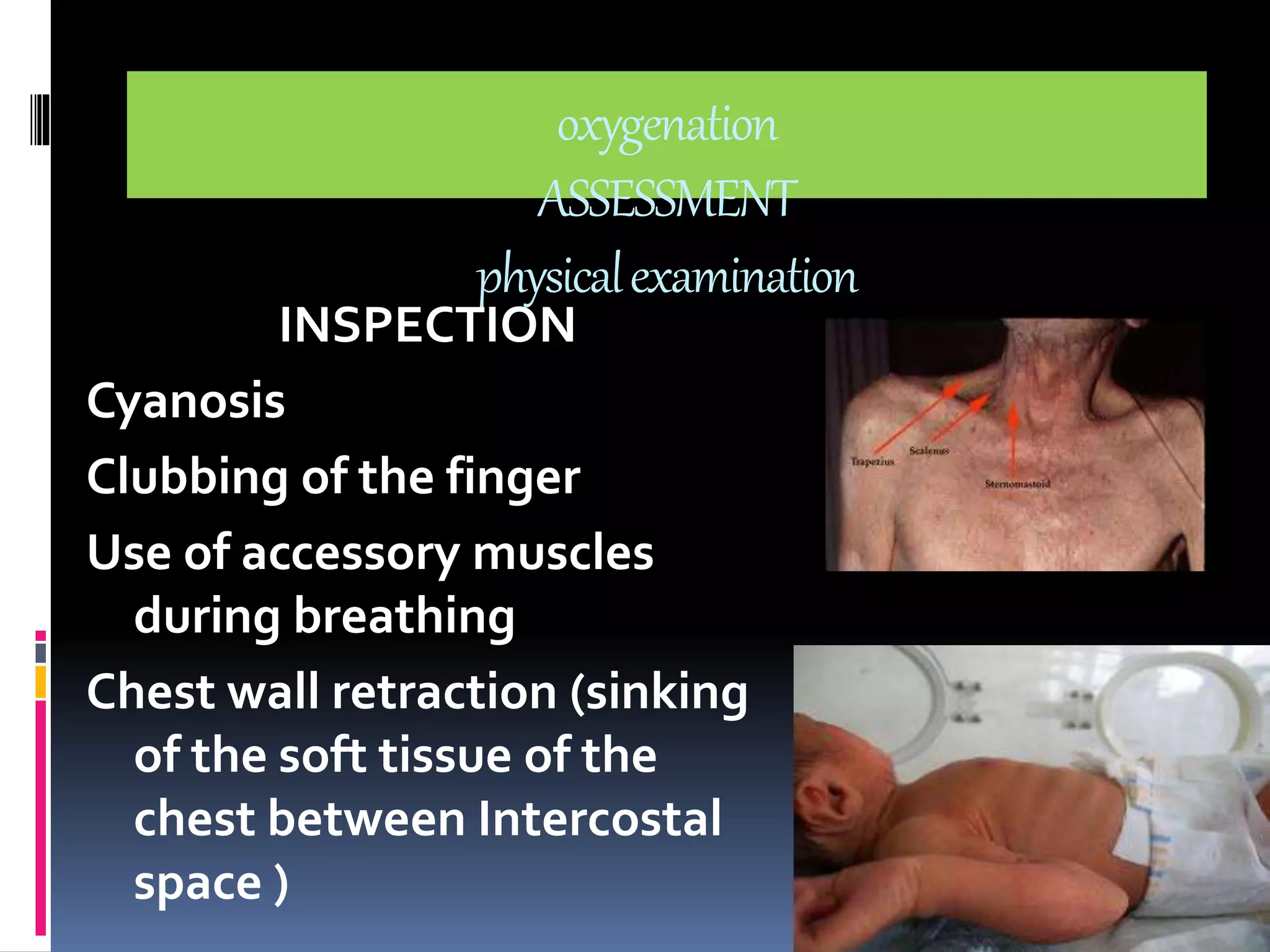
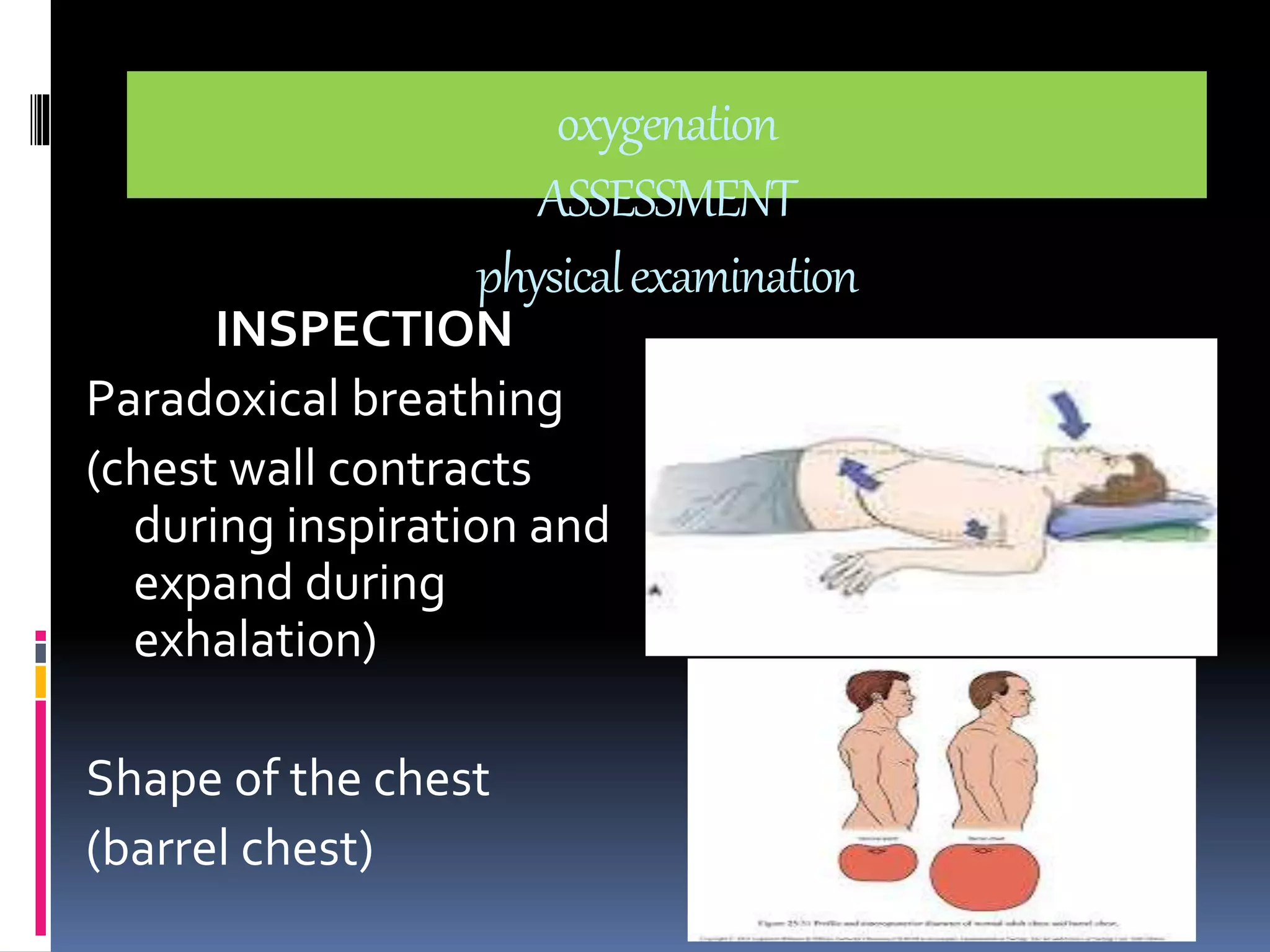
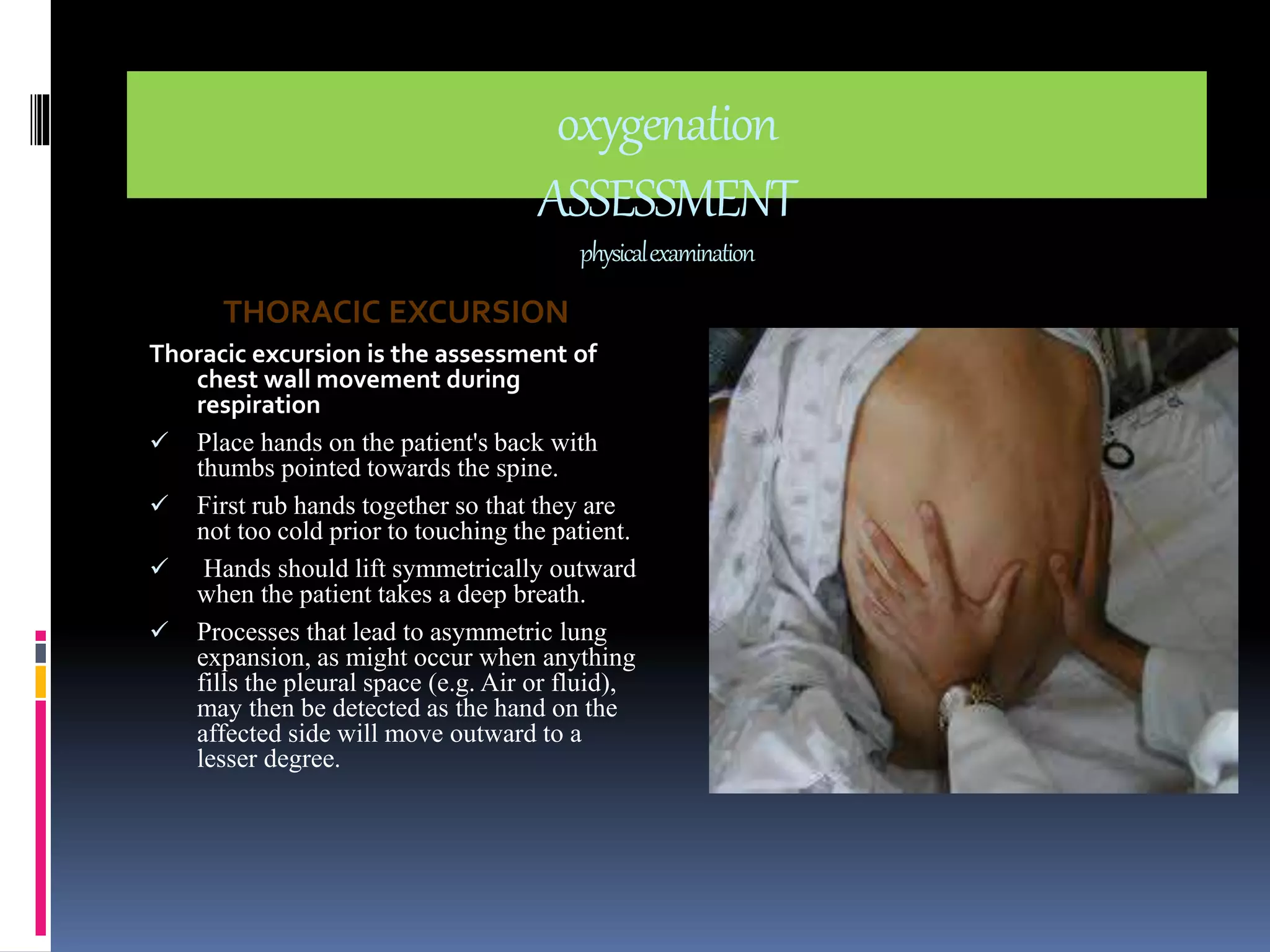
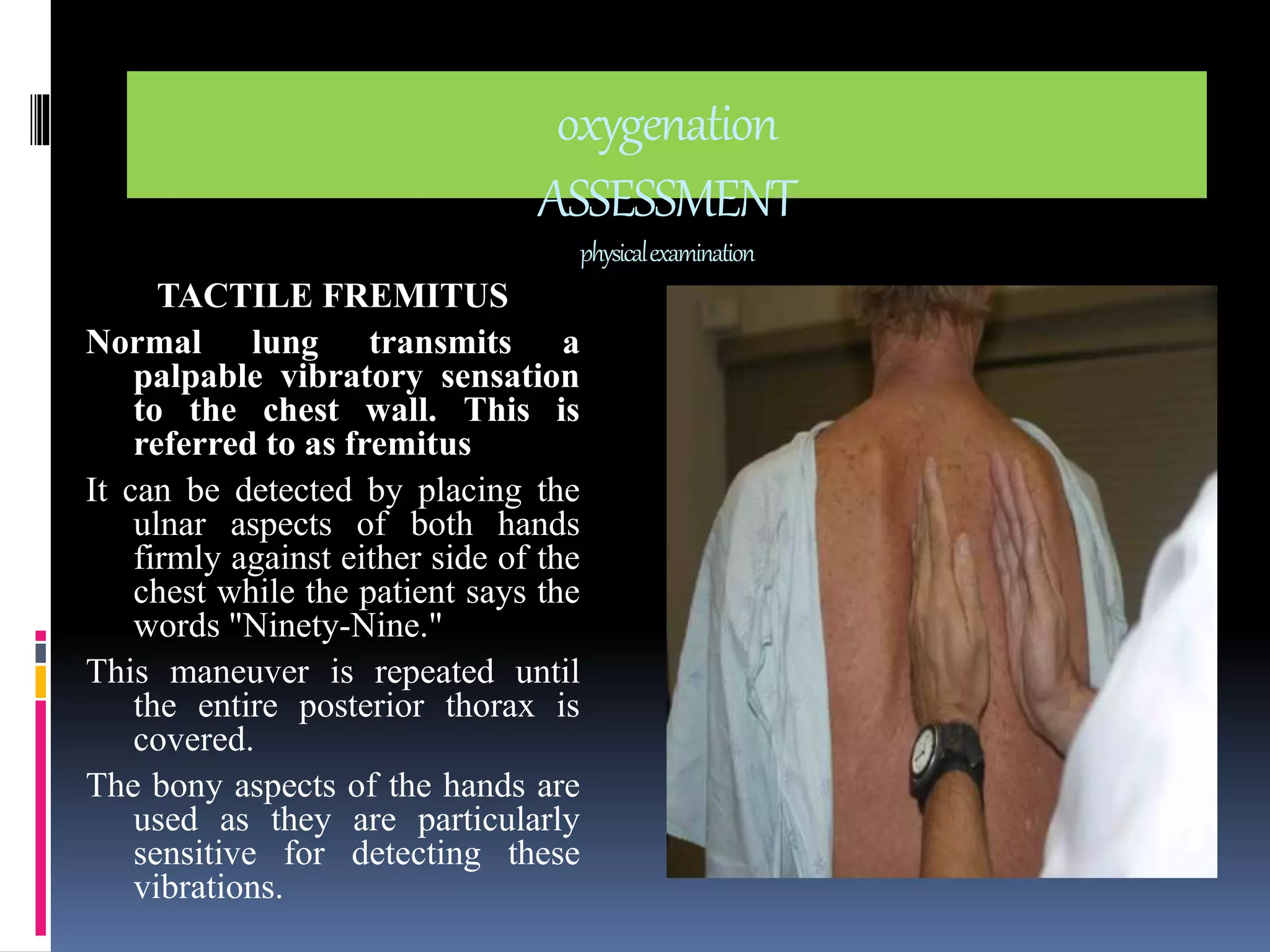
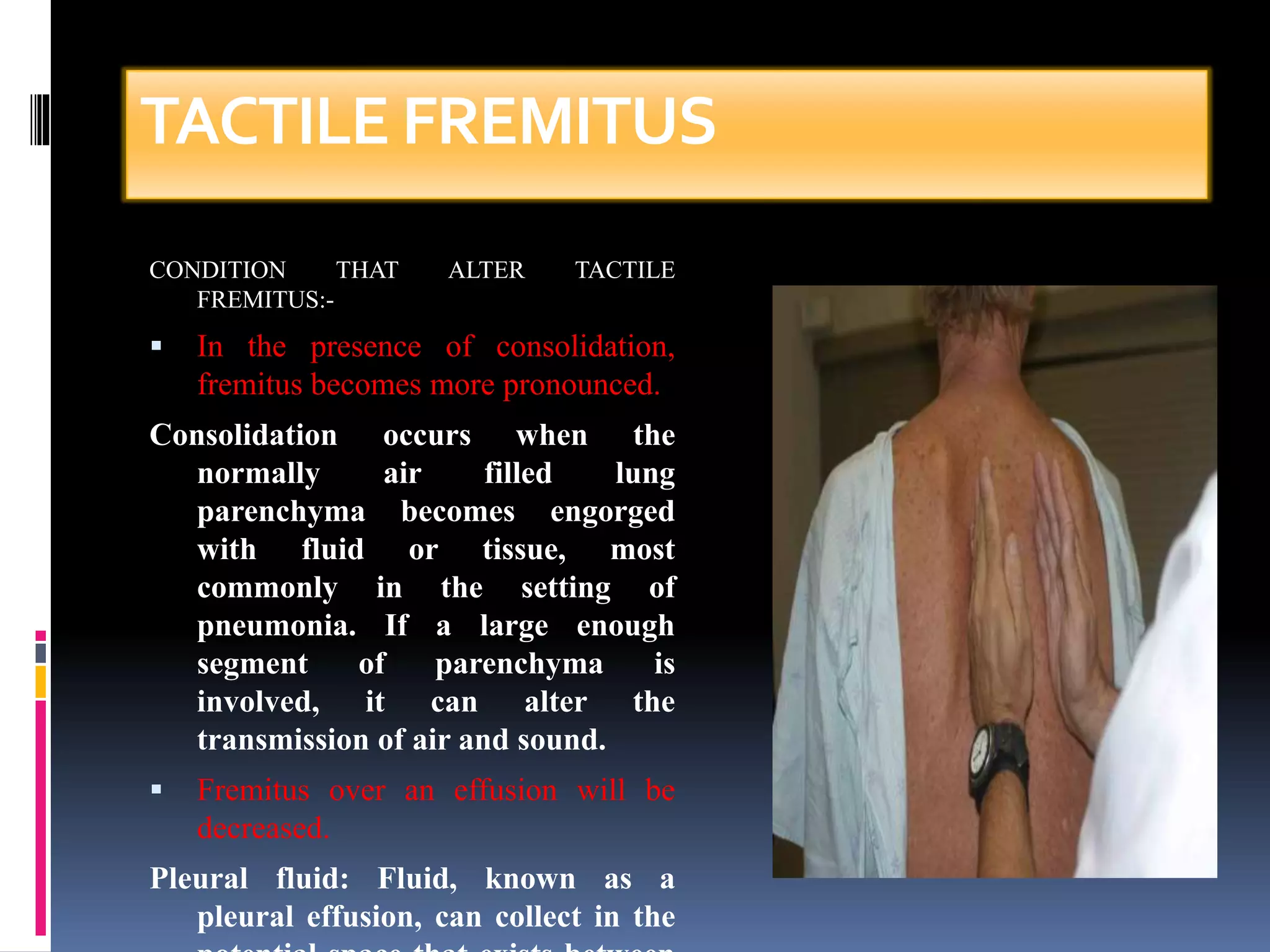
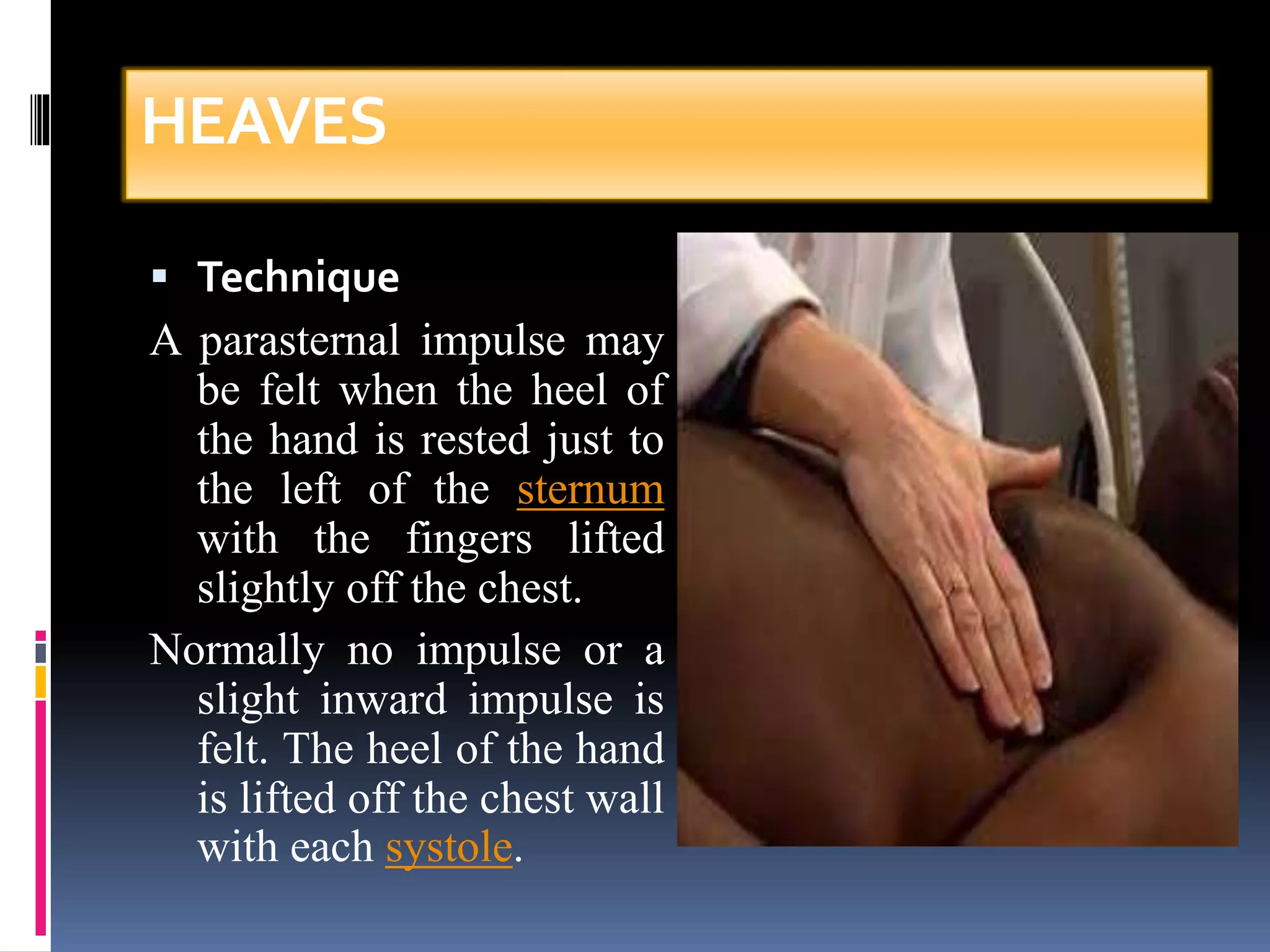
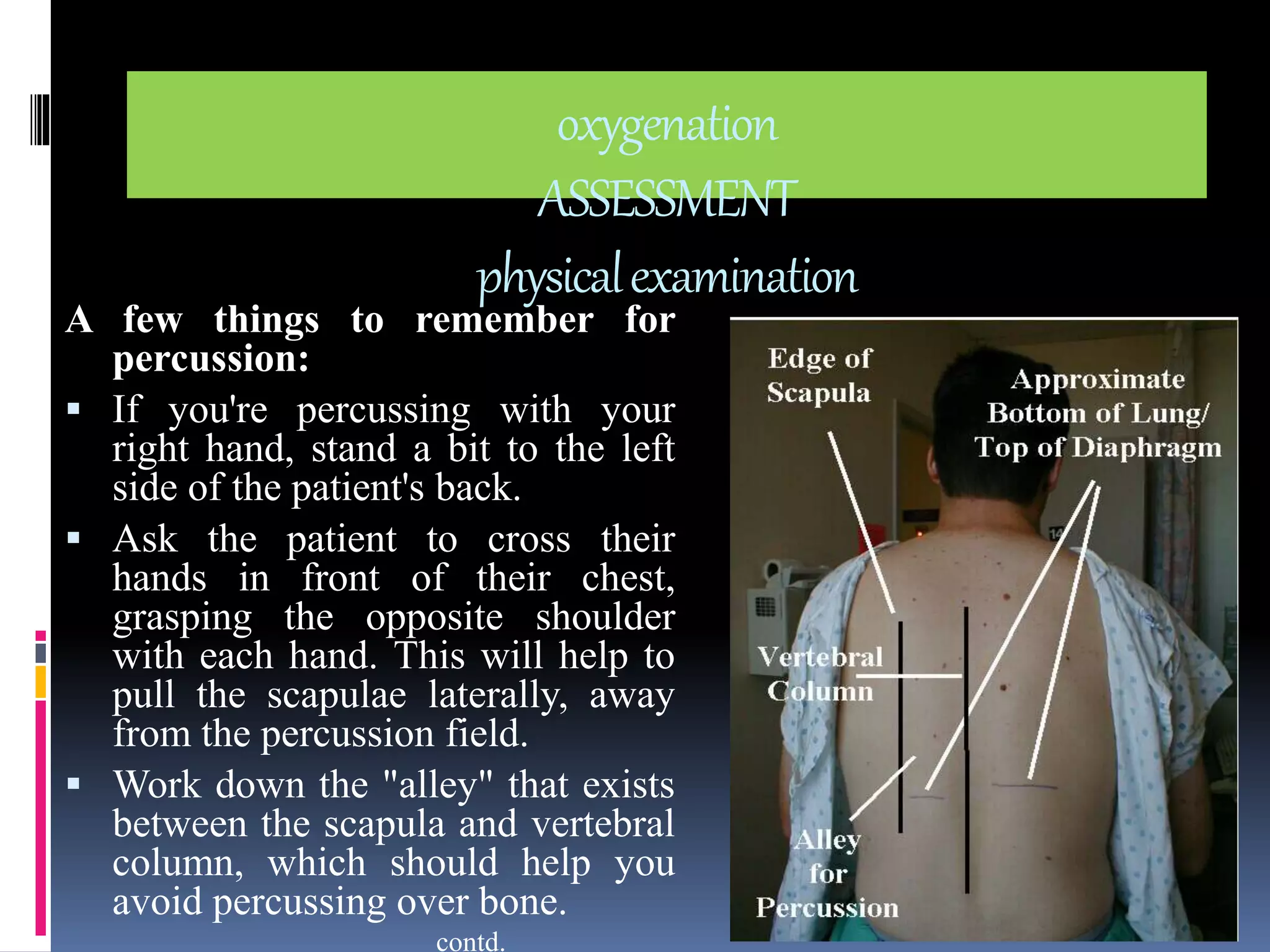
The document provides details on assessing a patient's oxygenation through nursing history, physical examination, and diagnostic tests. The nursing history focuses on collecting information on symptoms like chest pain, fatigue, dyspnea, cough, wheezing, respiratory infections, allergies, health risks, medications, smoking, and other exposures. The physical examination involves inspection of the skin, breathing patterns, and palpation techniques to examine thoracic excursion, tactile fremitus, thrills, and heaves.