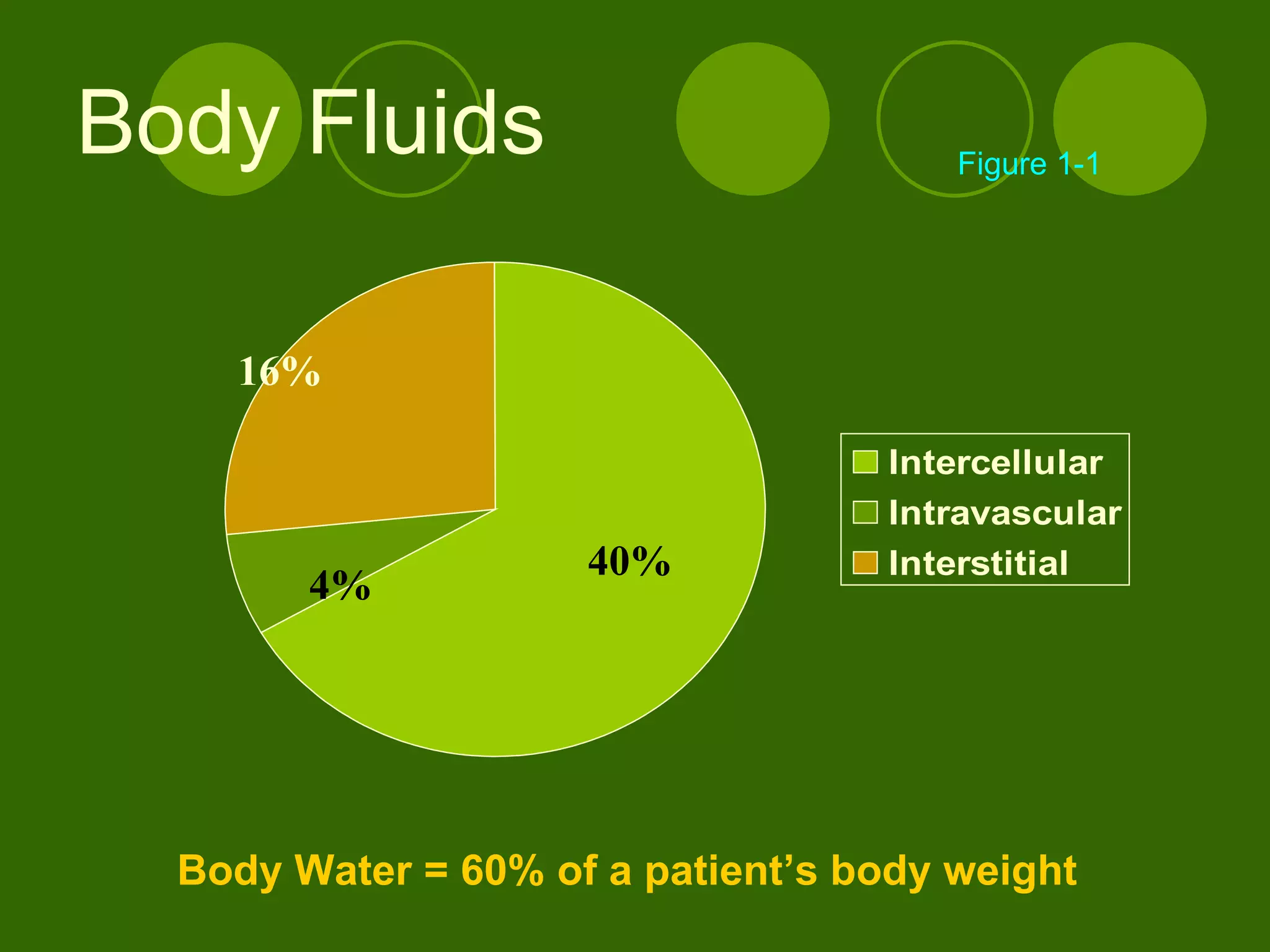
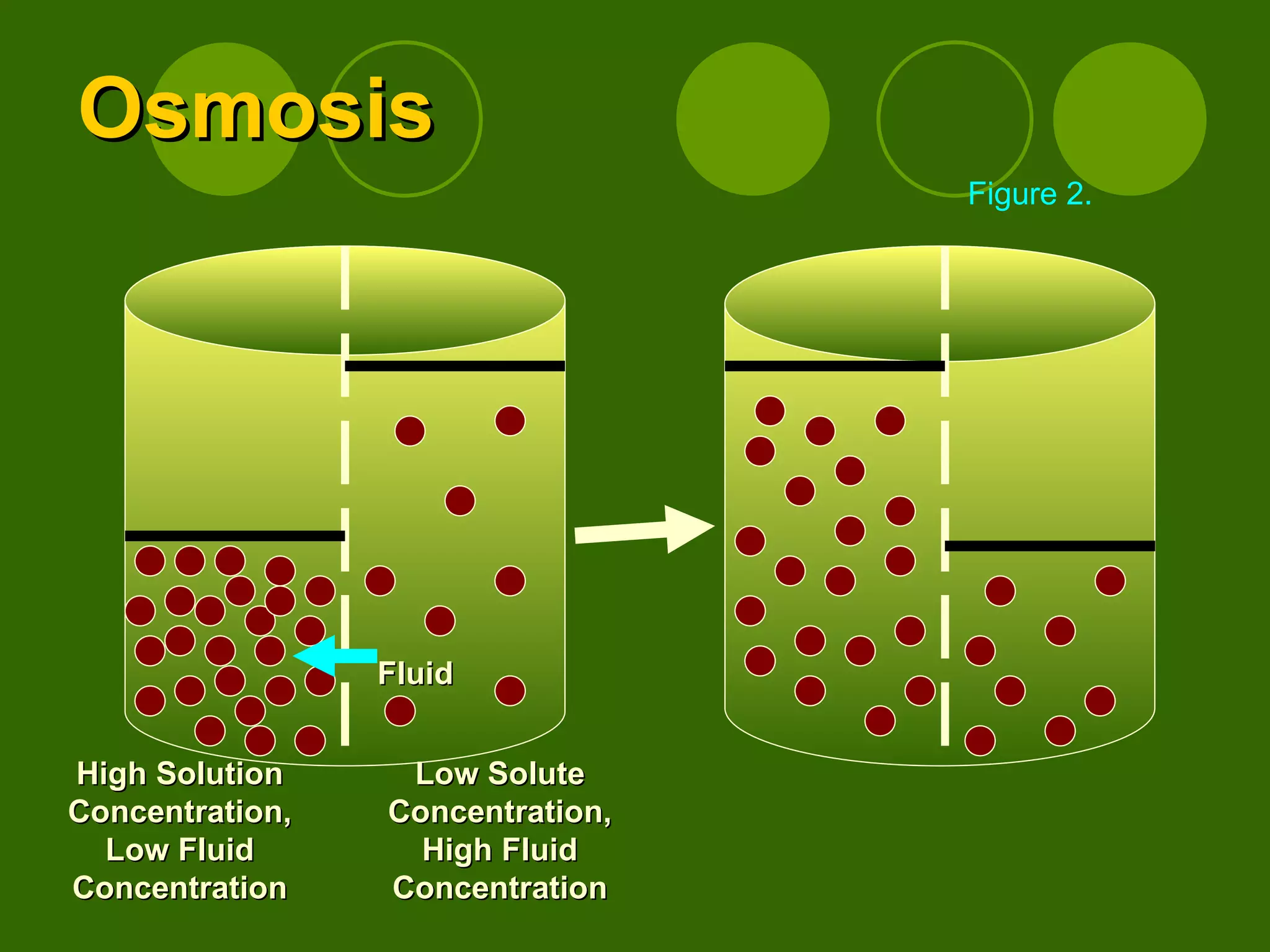
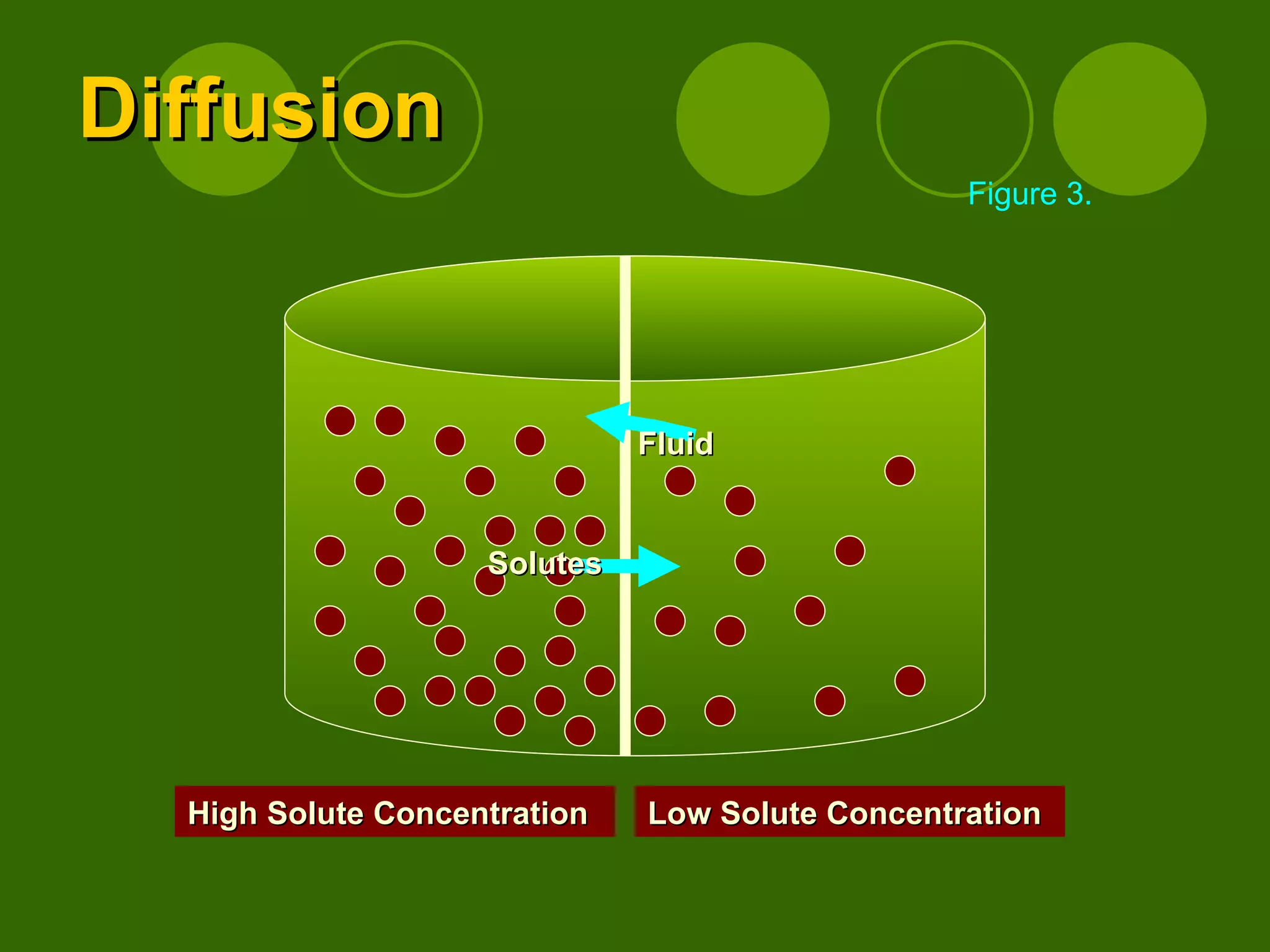
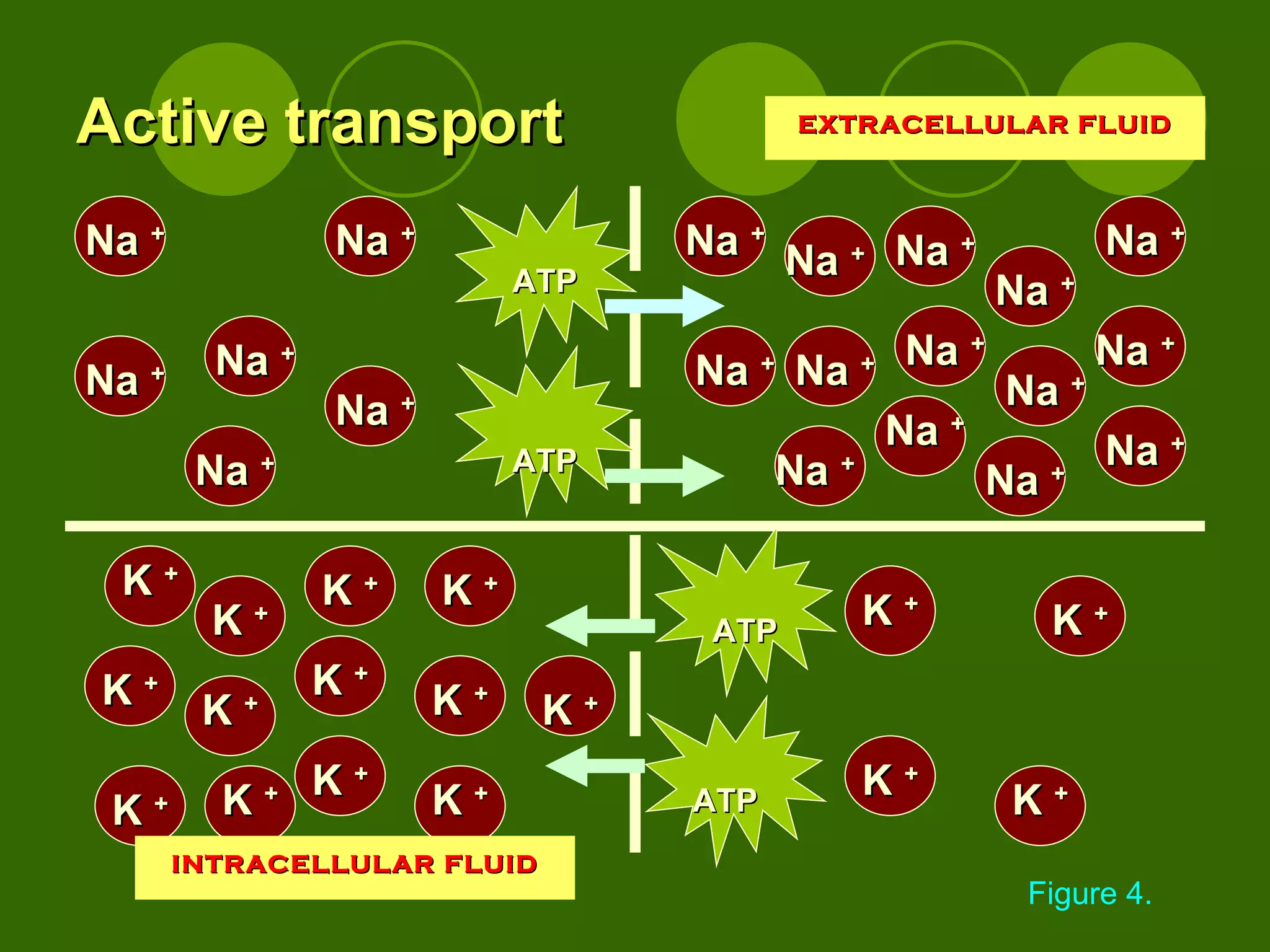
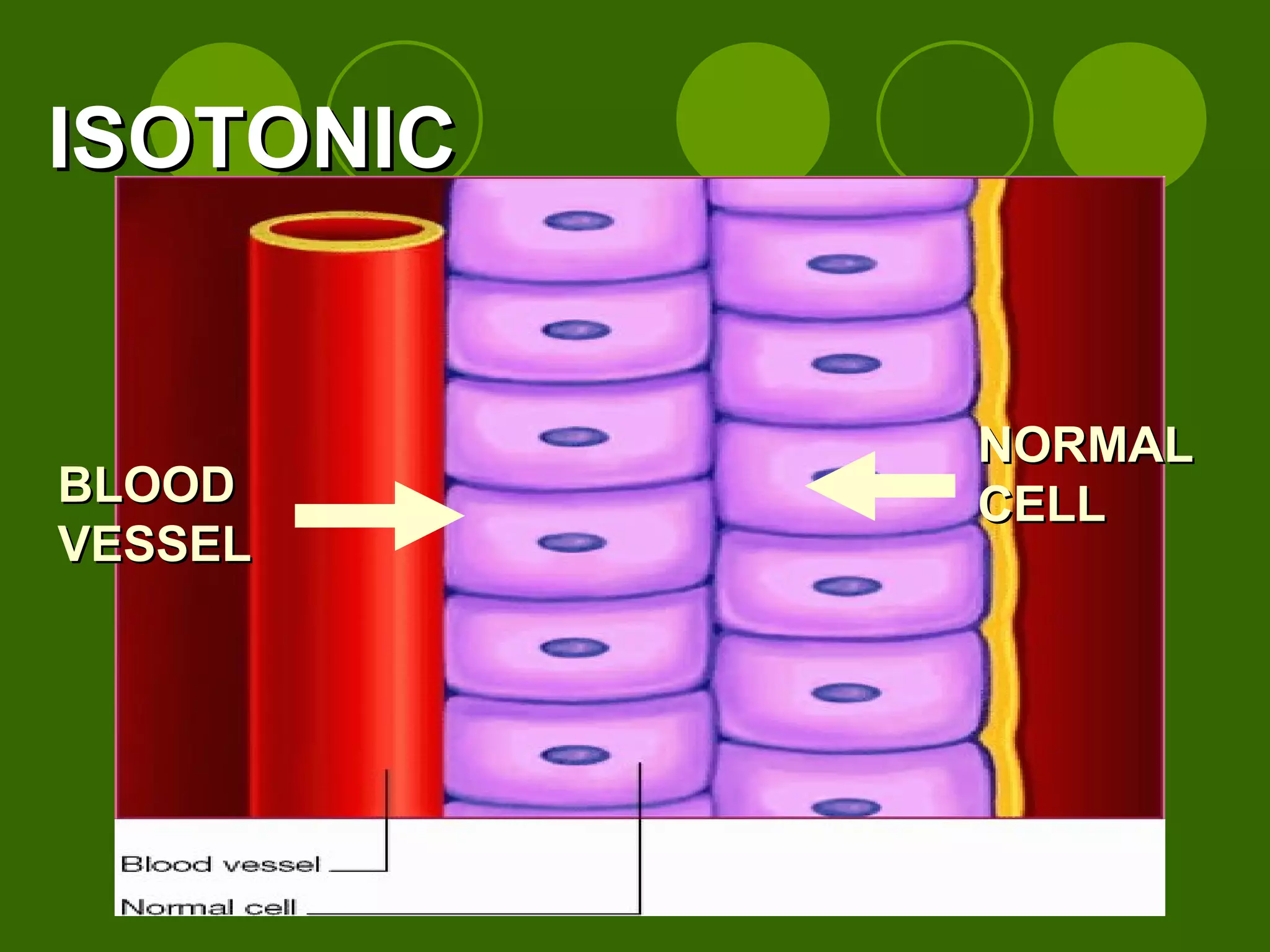
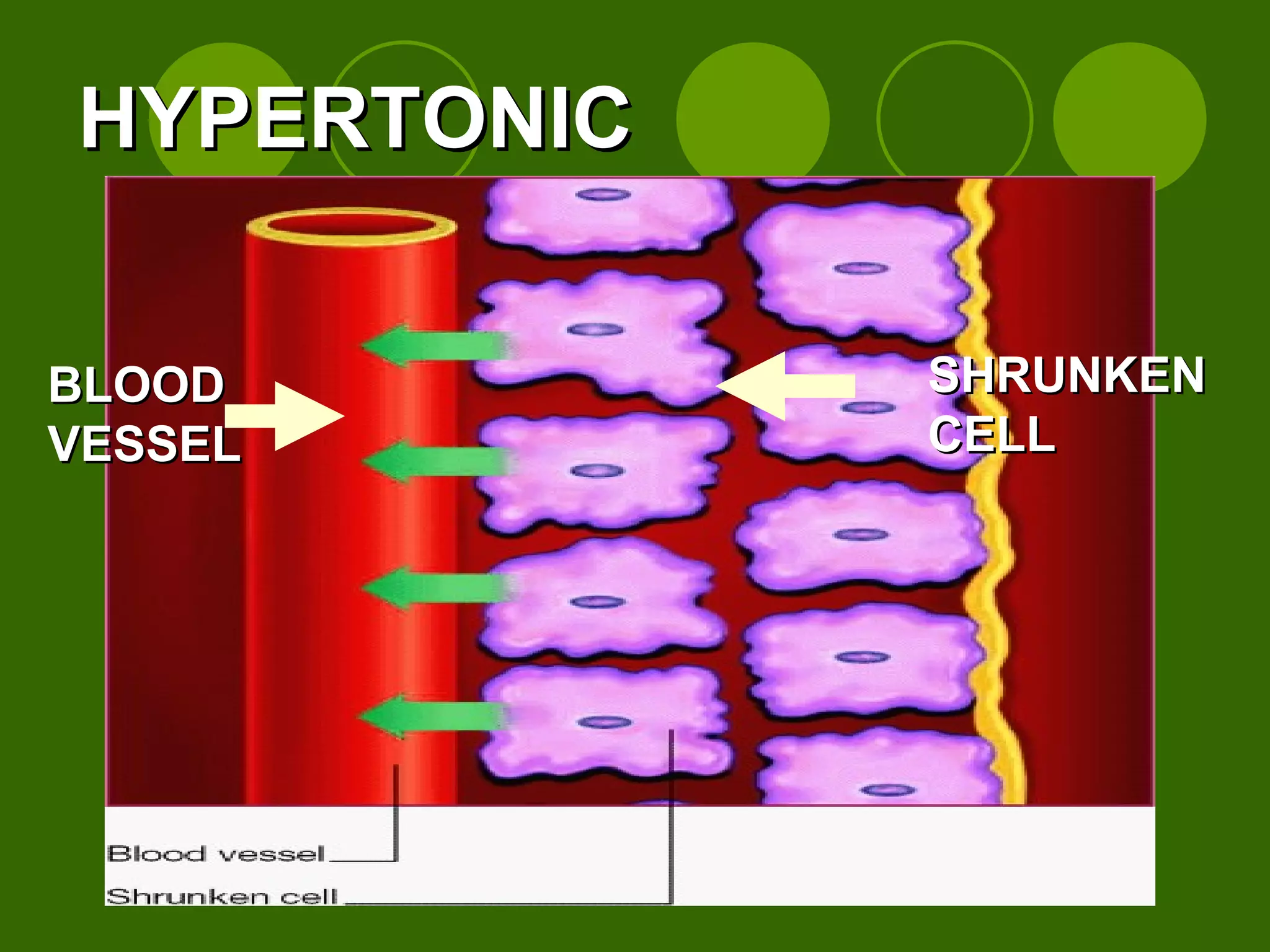
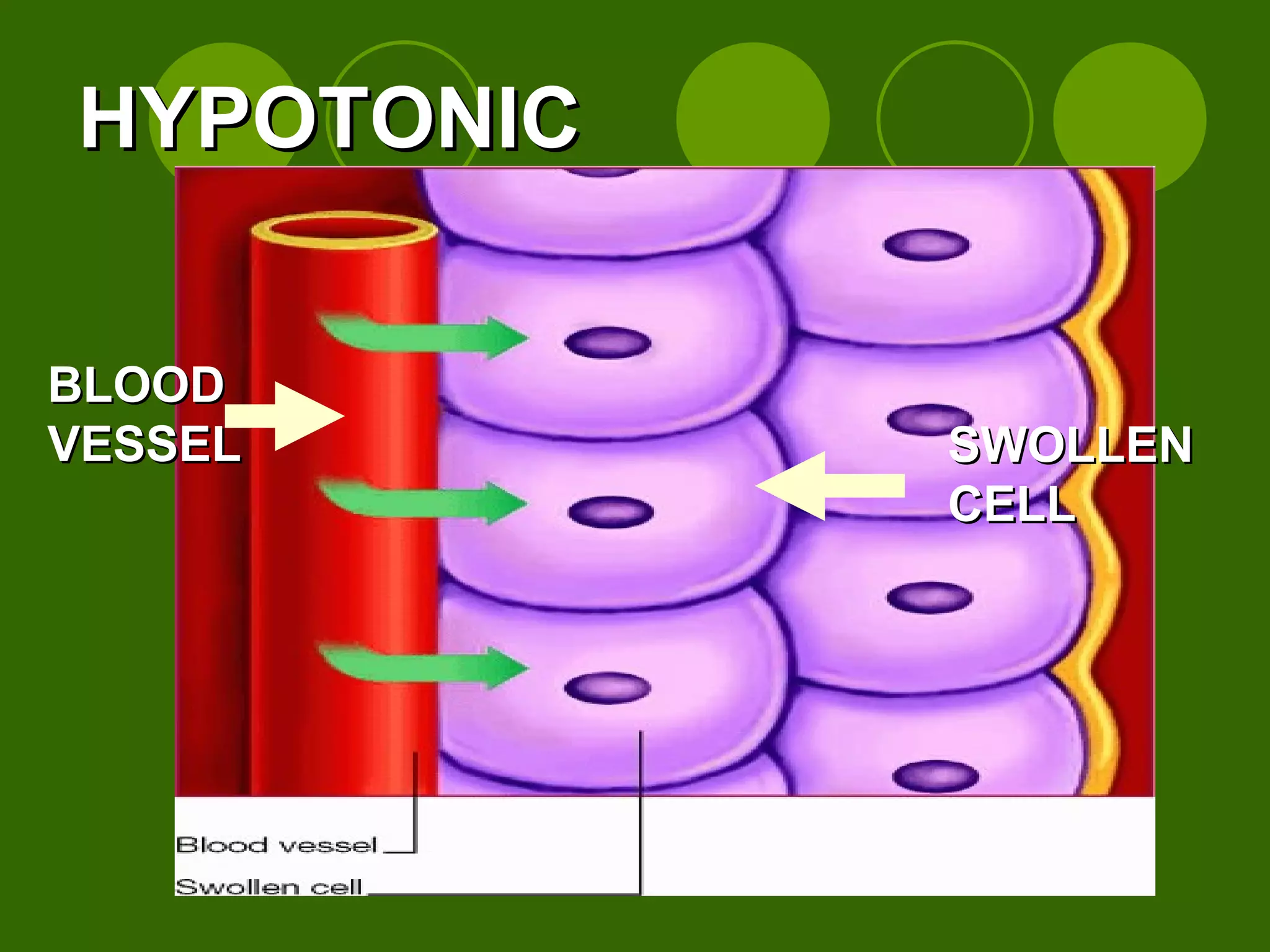
The document discusses fluid and electrolyte balance in the human body. It covers key topics like the components of body fluids, fluid compartments, electrolytes, fluid movement through diffusion, osmosis and active transport, causes of fluid shifts, effects of fluid imbalances, edema, and fluid resuscitation approaches.