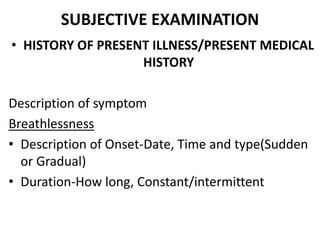
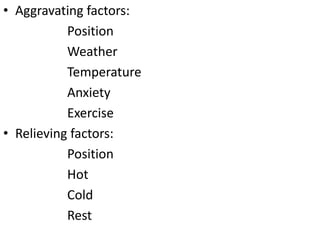
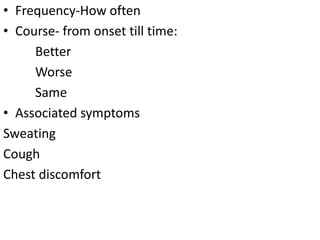
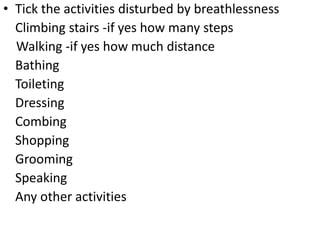
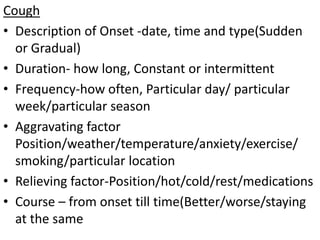
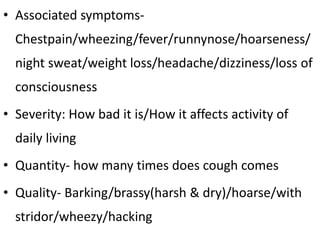
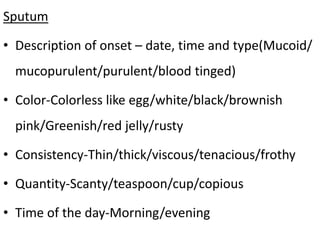
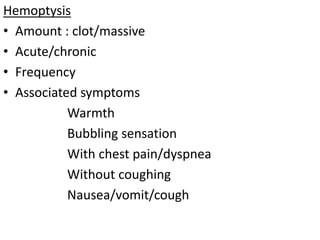
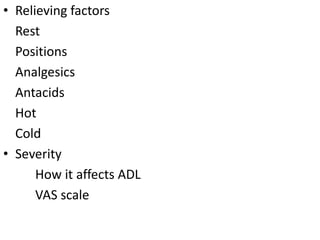
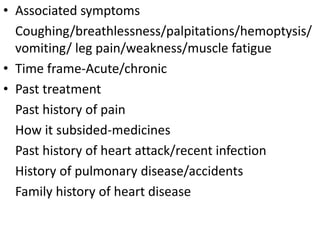
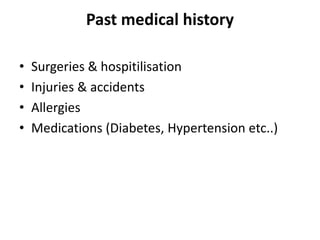
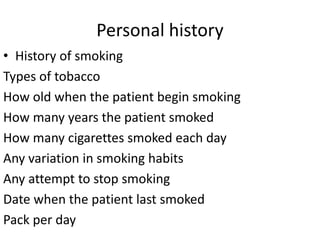
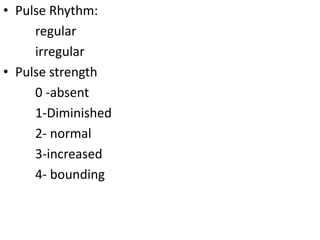
This document provides a template for conducting a cardio-respiratory assessment of a patient. It includes sections for collecting information on the patient's chief complaints, medical history, subjective examination involving the history of present illness and associated symptoms, as well as an objective examination involving vital signs, physical inspection, palpation, percussion, and auscultation of the chest, neck, and extremities. The assessment aims to gather comprehensive details on the patient's respiratory and cardiovascular health through a structured interview and physical exam.