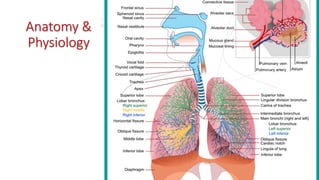
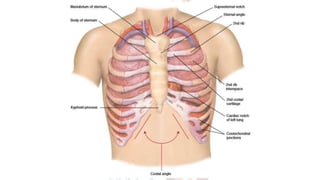
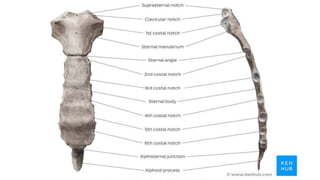
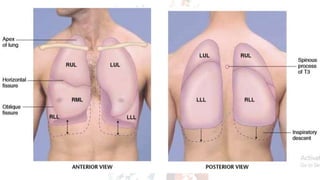
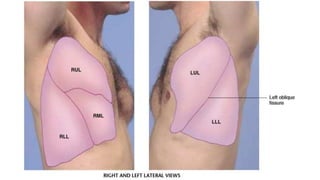
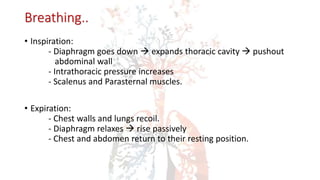
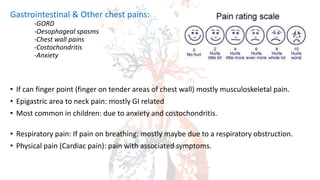
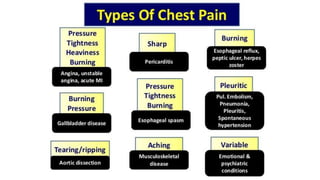
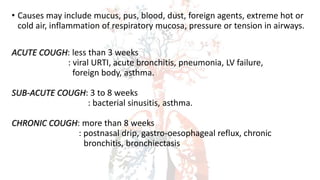
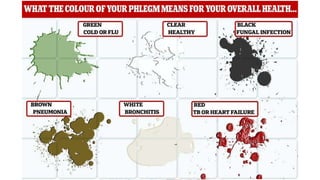
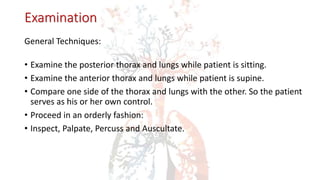
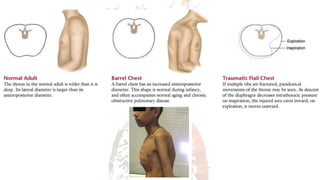
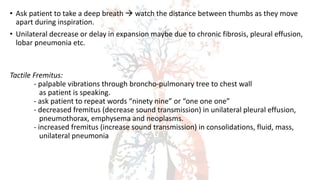
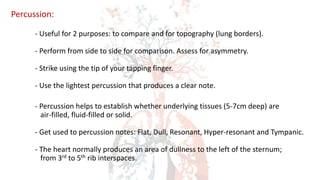
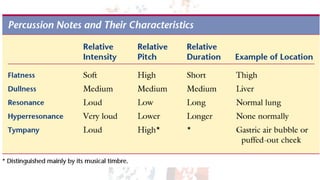
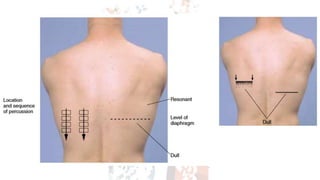
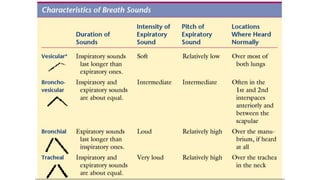
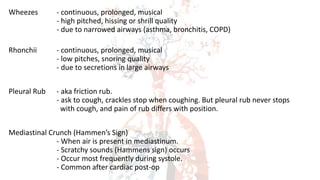
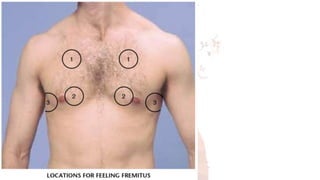
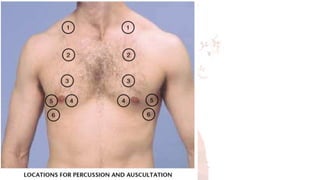
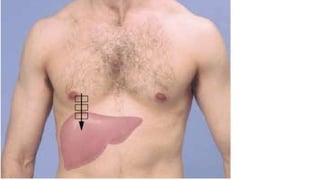
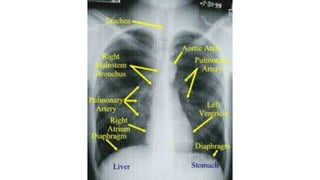
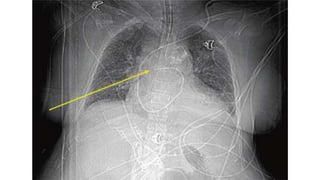
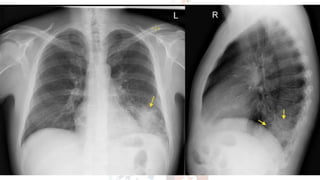
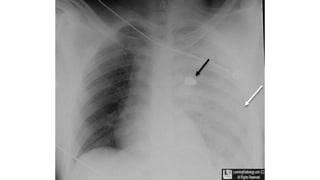
This document provides an overview of the anatomy and physiology of the respiratory system. It discusses the structure of the lungs including lobes and fissures. It describes the trachea and bronchi. It explains the mechanics of breathing including inspiration and expiration. It discusses how to assess common respiratory symptoms like cough, wheezing, shortness of breath, and hemoptysis through patient history. It outlines the examination of the respiratory system including inspection, palpation, percussion, and auscultation of the chest. Adventitious breath sounds like rales, rhonchi, and wheezes are also described.