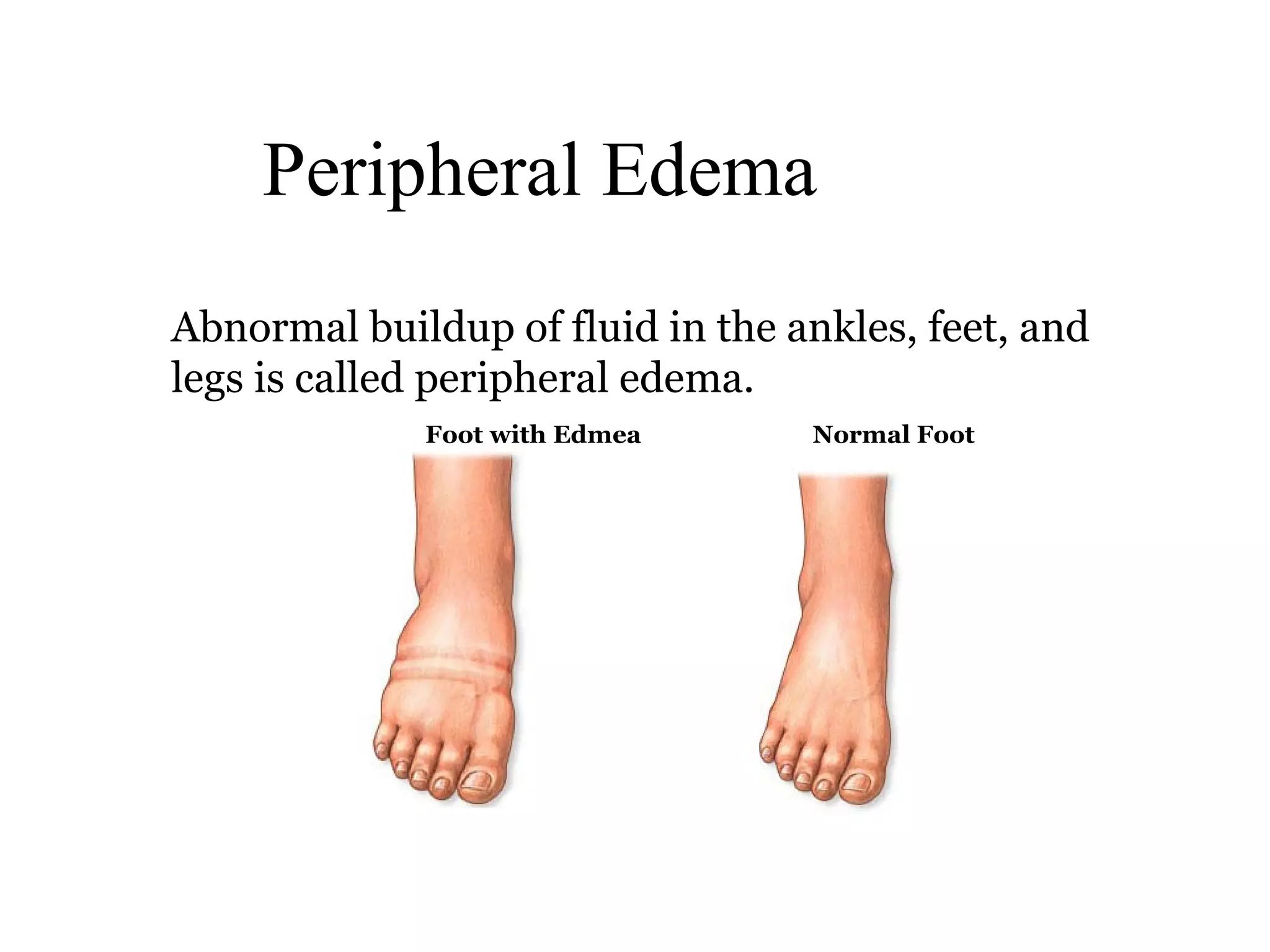
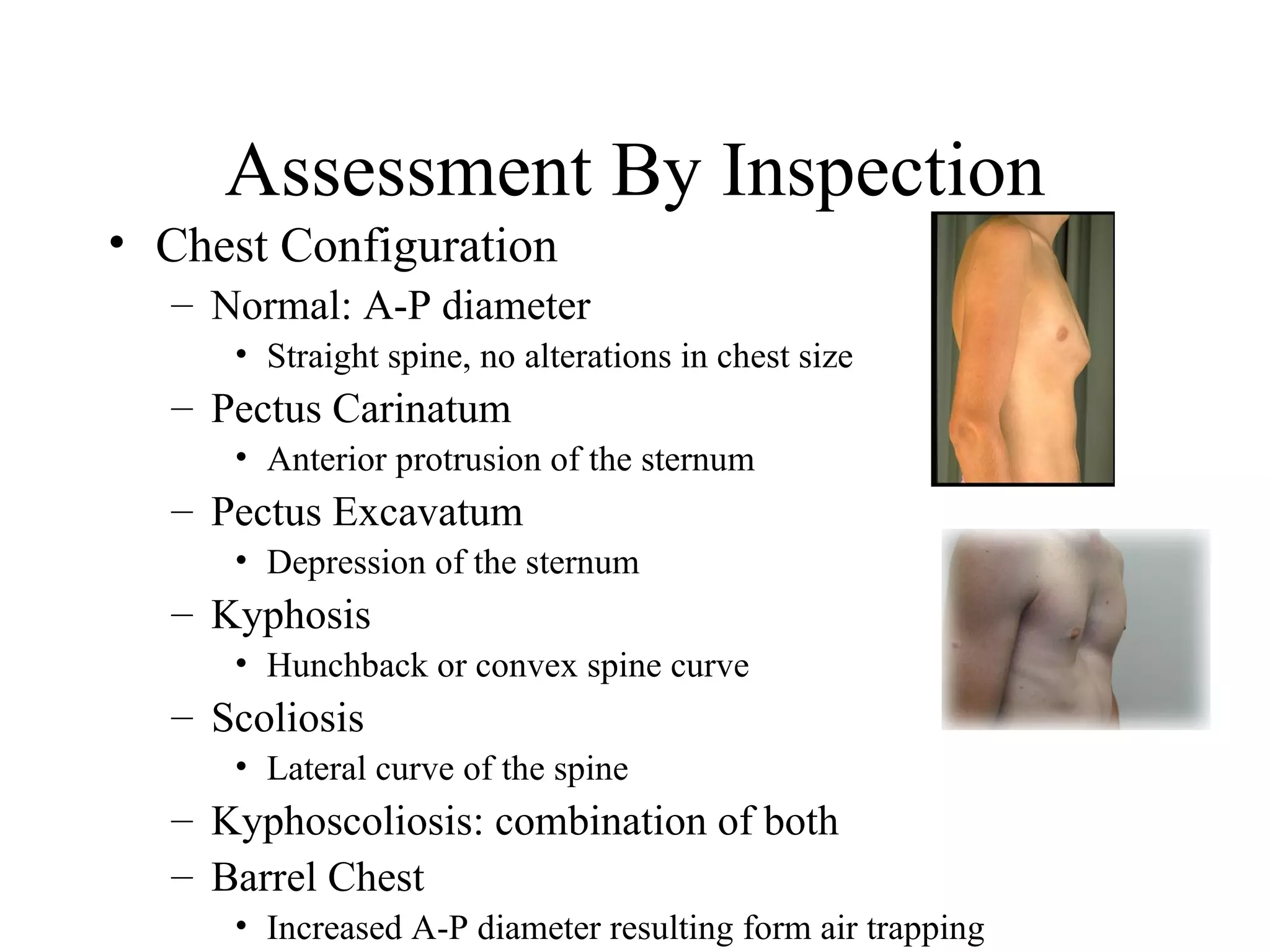
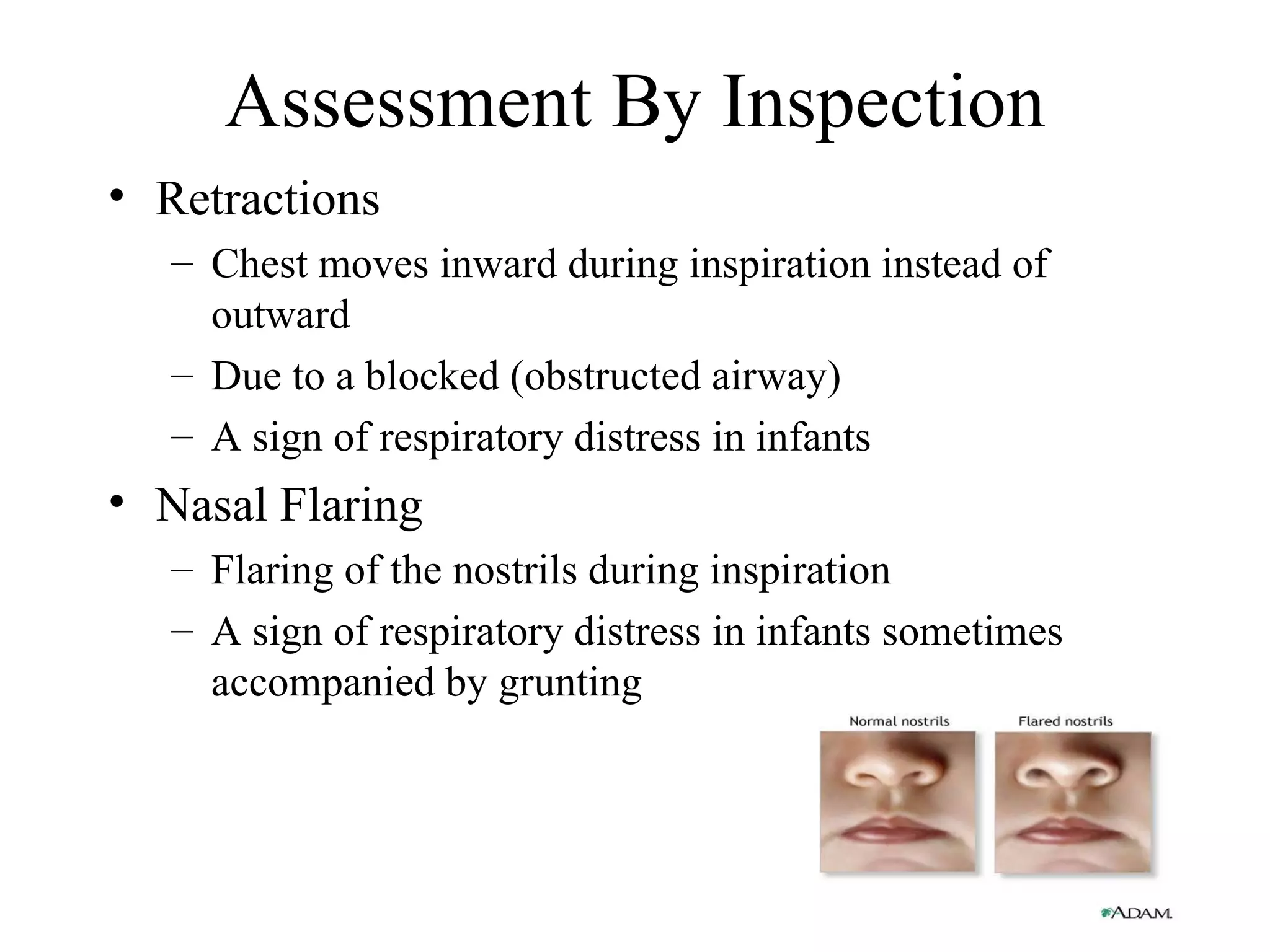
This document provides information on conducting an assessment of a patient, including the importance of conducting a patient interview and physical examination. It outlines the major components of a patient interview, such as determining level of consciousness, orientation, emotional state, subjective symptoms, and medical history. It also describes techniques for conducting a physical examination, including inspection of general appearance and specific areas, palpation of pulses and chest, percussion, and auscultation of breath sounds. The overall goal of the assessment is to obtain an initial and secondary evaluation of the patient through interview and examination.