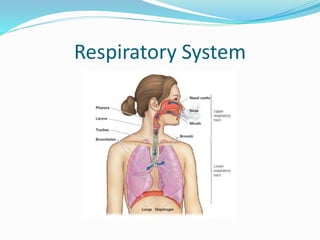
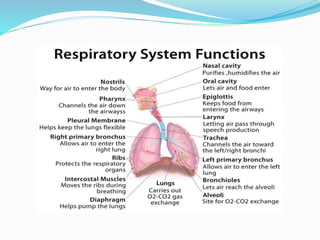
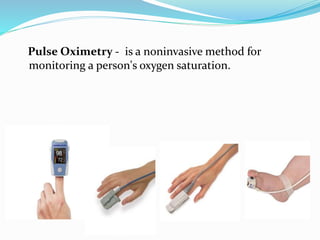
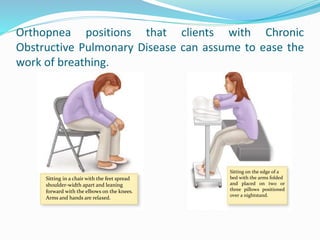
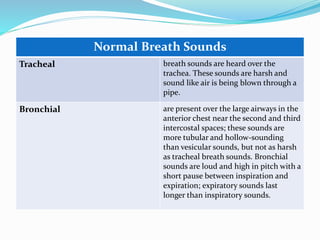
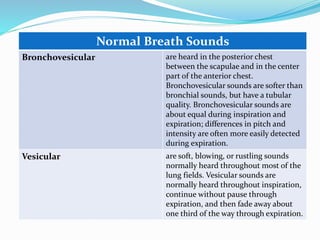
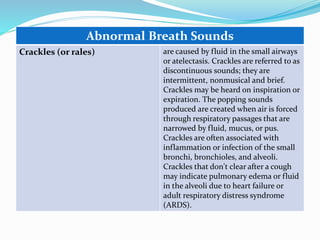
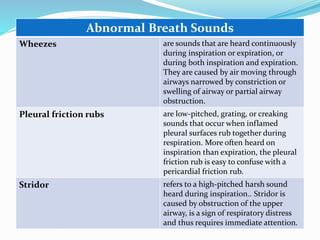
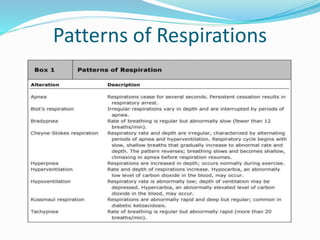
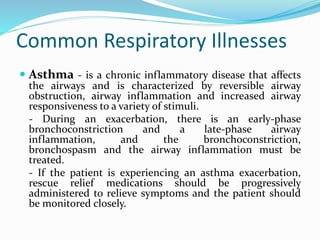
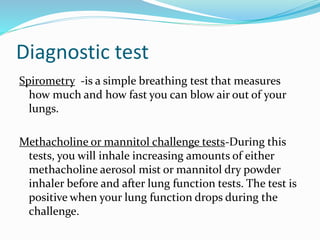
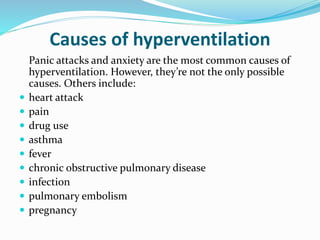
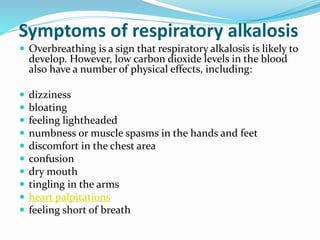
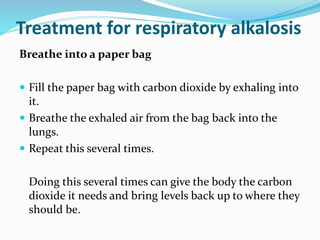
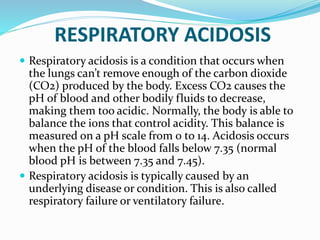
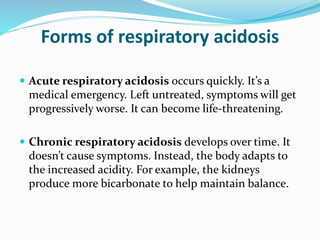
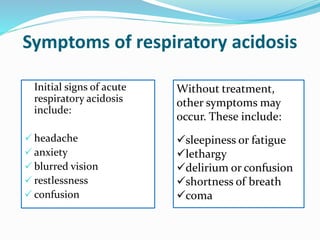
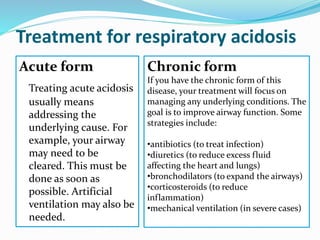
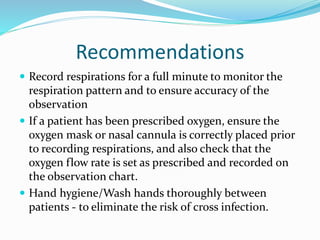
This document provides information on performing a respiratory assessment, including objectives, the process of respiratory assessment, signs and symptoms to assess for, abnormal breath sounds, and common respiratory illnesses like asthma, pneumonia, COPD, and respiratory acidosis and alkalosis. The key steps are to inspect the chest, auscultate breath sounds, assess rate and effort, document findings, and understand common diseases and treatments.