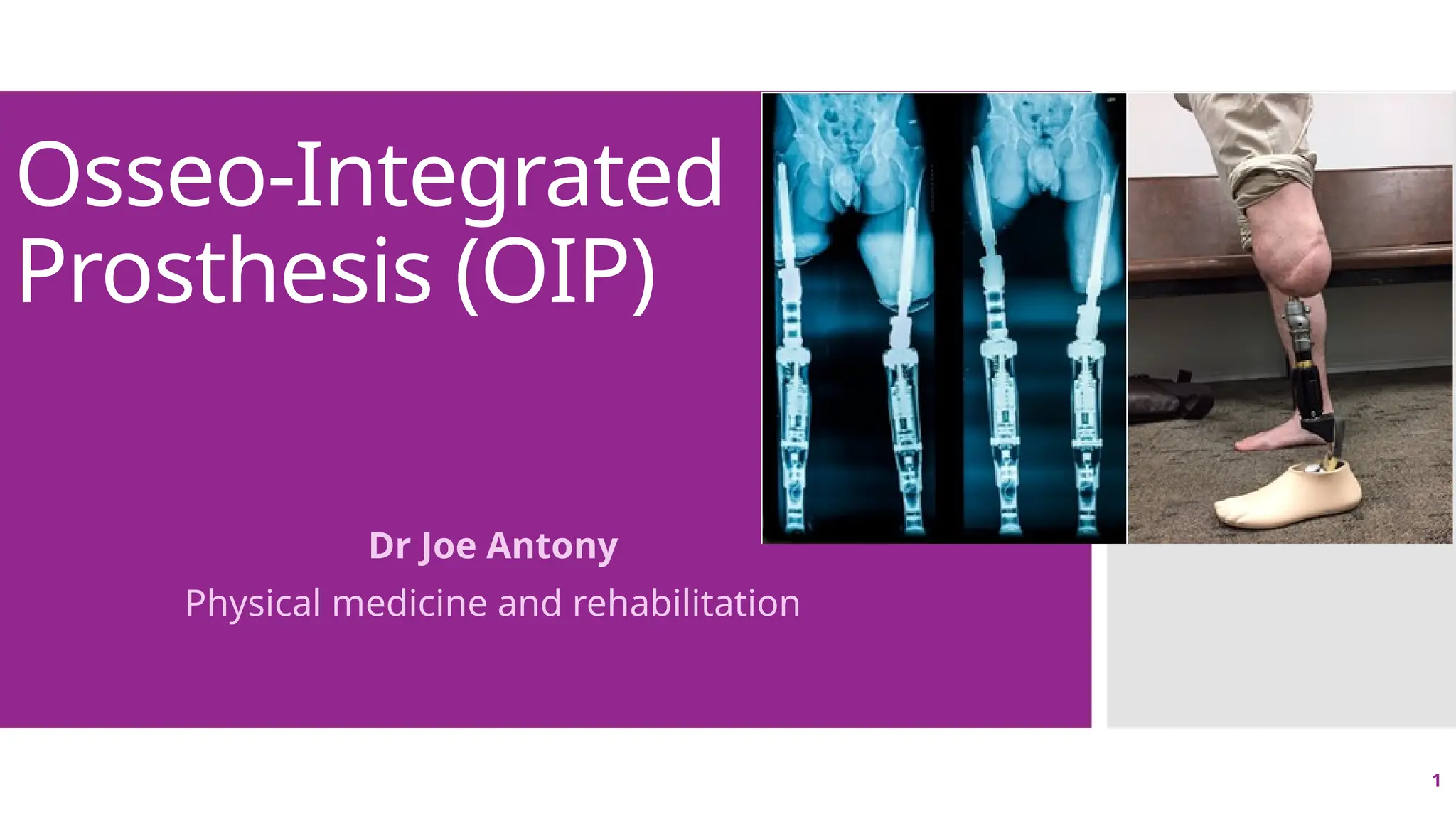
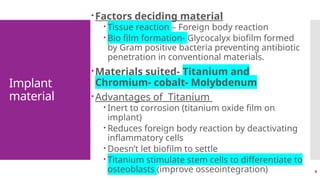
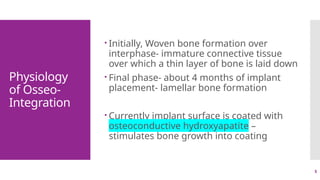
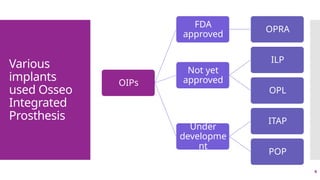
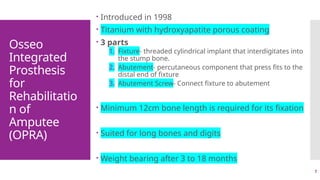
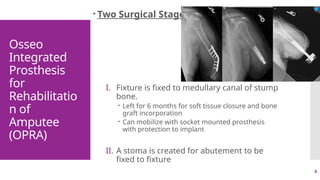
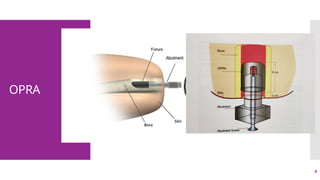
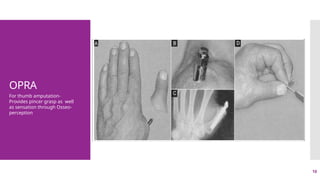
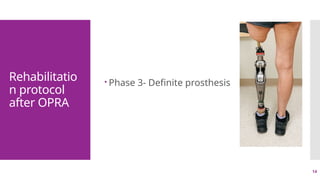
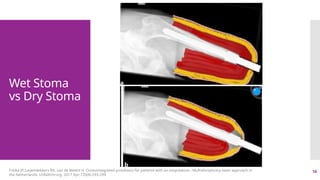
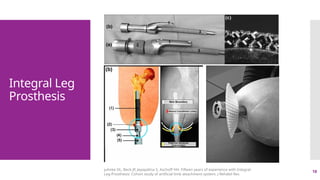
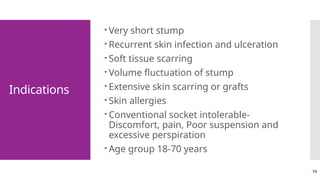
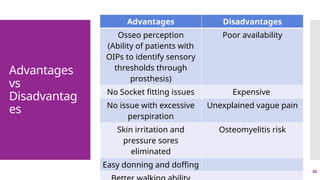
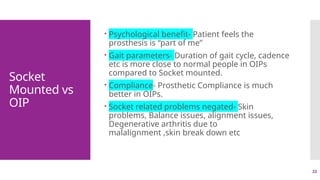
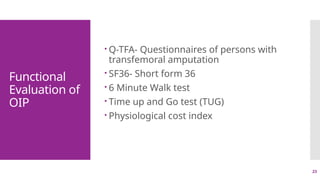
The document discusses osseo-integrated prostheses (OIPs), which are external prosthetics attached to the skeleton through osseointegration, outlining their design, implant materials, physiology, and rehabilitation protocols. It also covers advantages, disadvantages, contraindications, and functional evaluation of OIPs, along with future directions in research. Key aspects include the management of amputees with specific requirements and the implications of osseo-perception in improving prosthetic functionality.