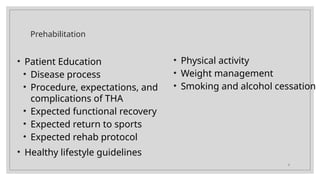
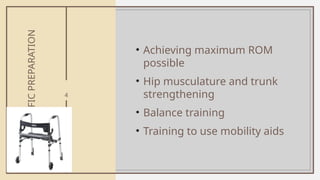
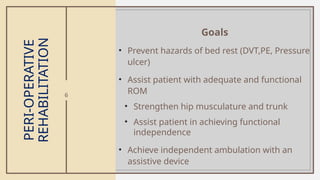
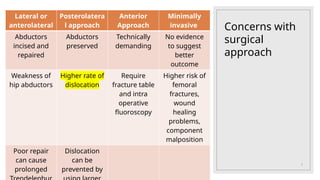
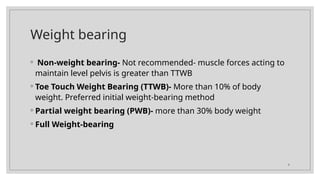
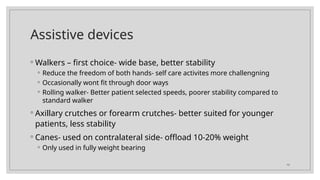
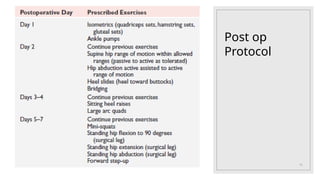
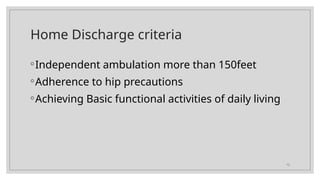
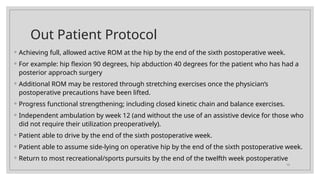
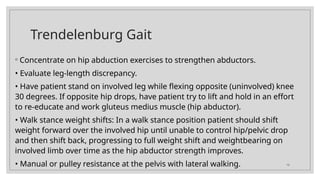
The document outlines the rehabilitation process following total hip replacement, covering prehabilitation, surgical approaches, and post-operative care. It emphasizes patient education, functional recovery goals, weight-bearing protocols, assistive devices, and guidelines for achieving maximum range of motion and independence. Complications and common rehabilitation issues, such as gait deviations and flexion contractures, are also addressed, along with specific exercises and precautions to ensure the best recovery outcomes.