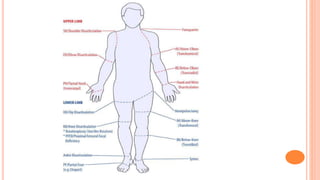
The document provides an overview of general principles and techniques for amputation. It discusses:
1. The definition of amputation and its historical development from ancient times to modern antiseptic techniques.
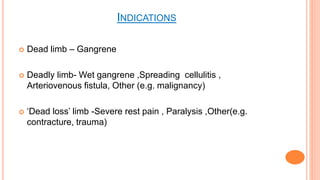
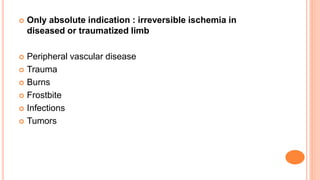
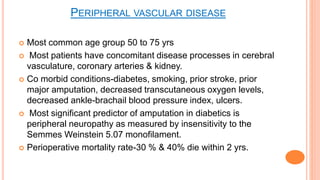
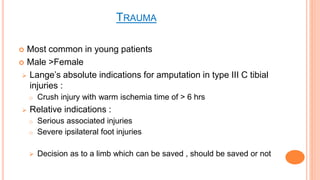
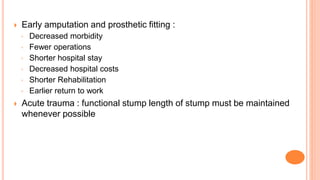
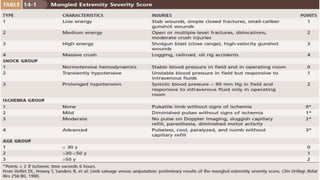
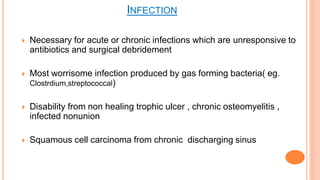
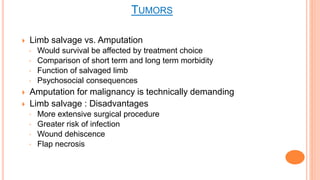
2. The common indications for amputation including peripheral vascular disease, trauma, infections, and tumors.
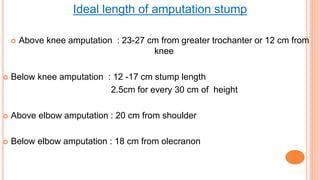
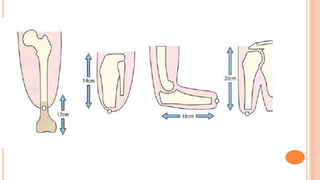
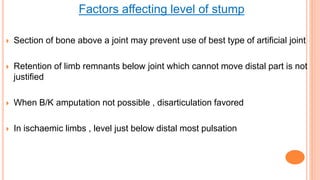
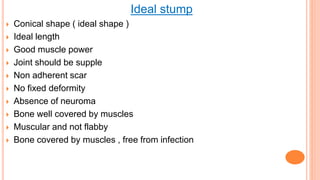
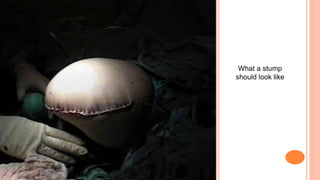
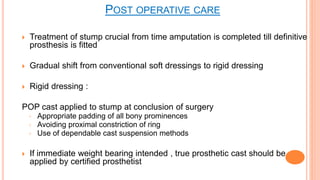
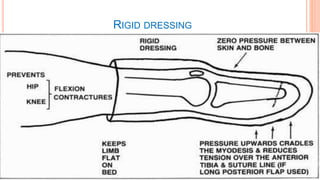
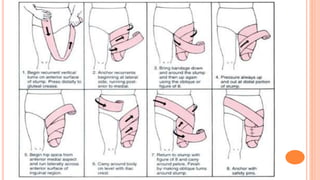
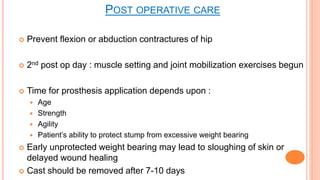
3. Surgical principles such as ideal stump shape and length, techniques for blood vessels, nerves, muscles and bone, and postoperative care including rigid dressings.
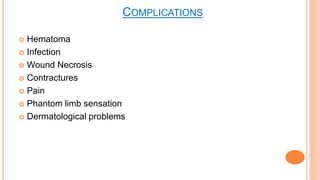
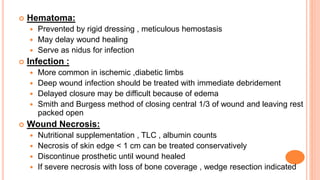
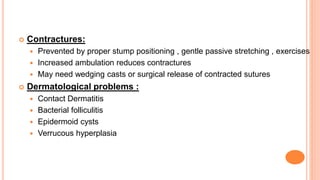
4. Potential complications like hematoma, infection, wound necrosis, contractures and phantom limb pain.