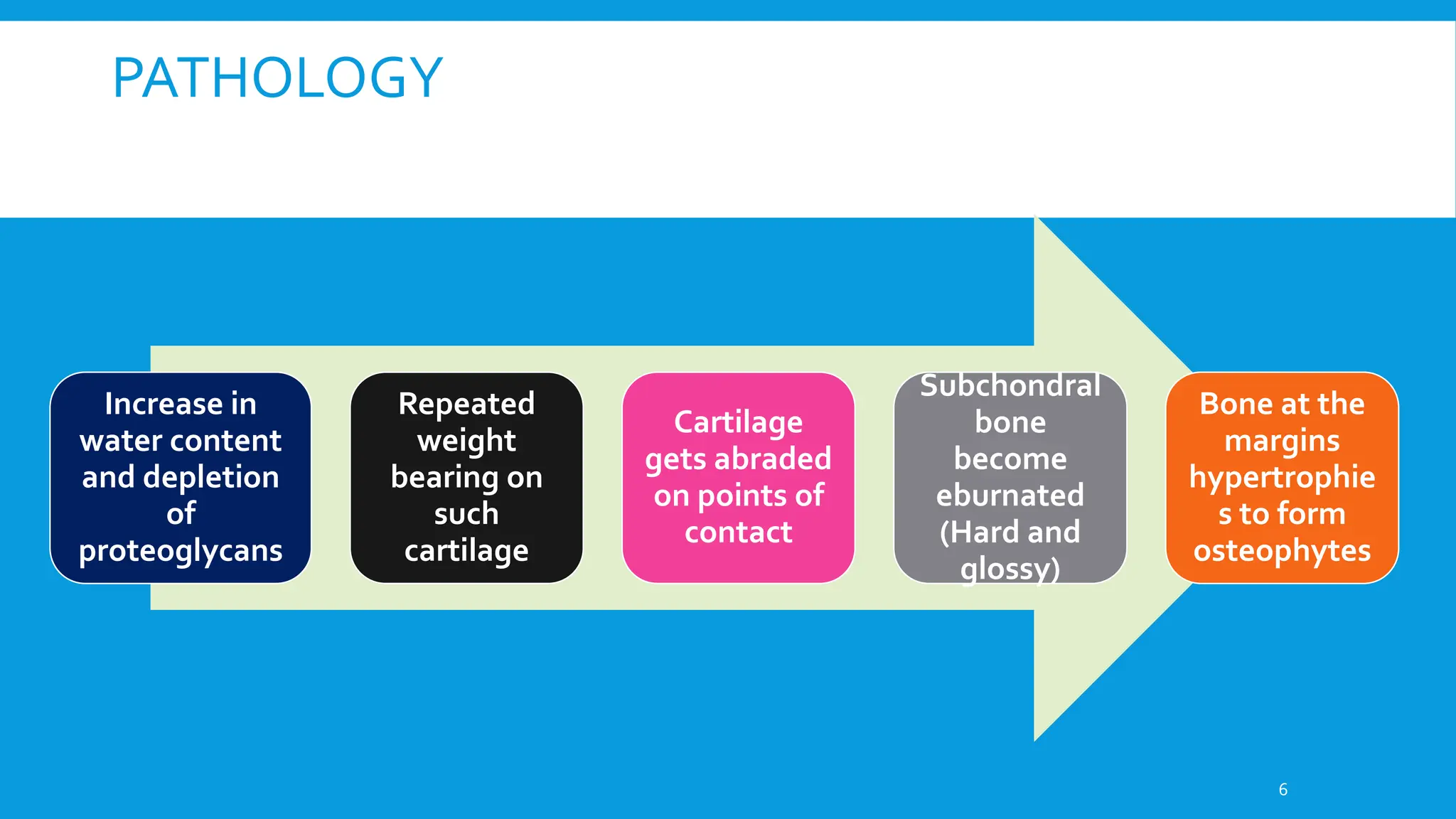
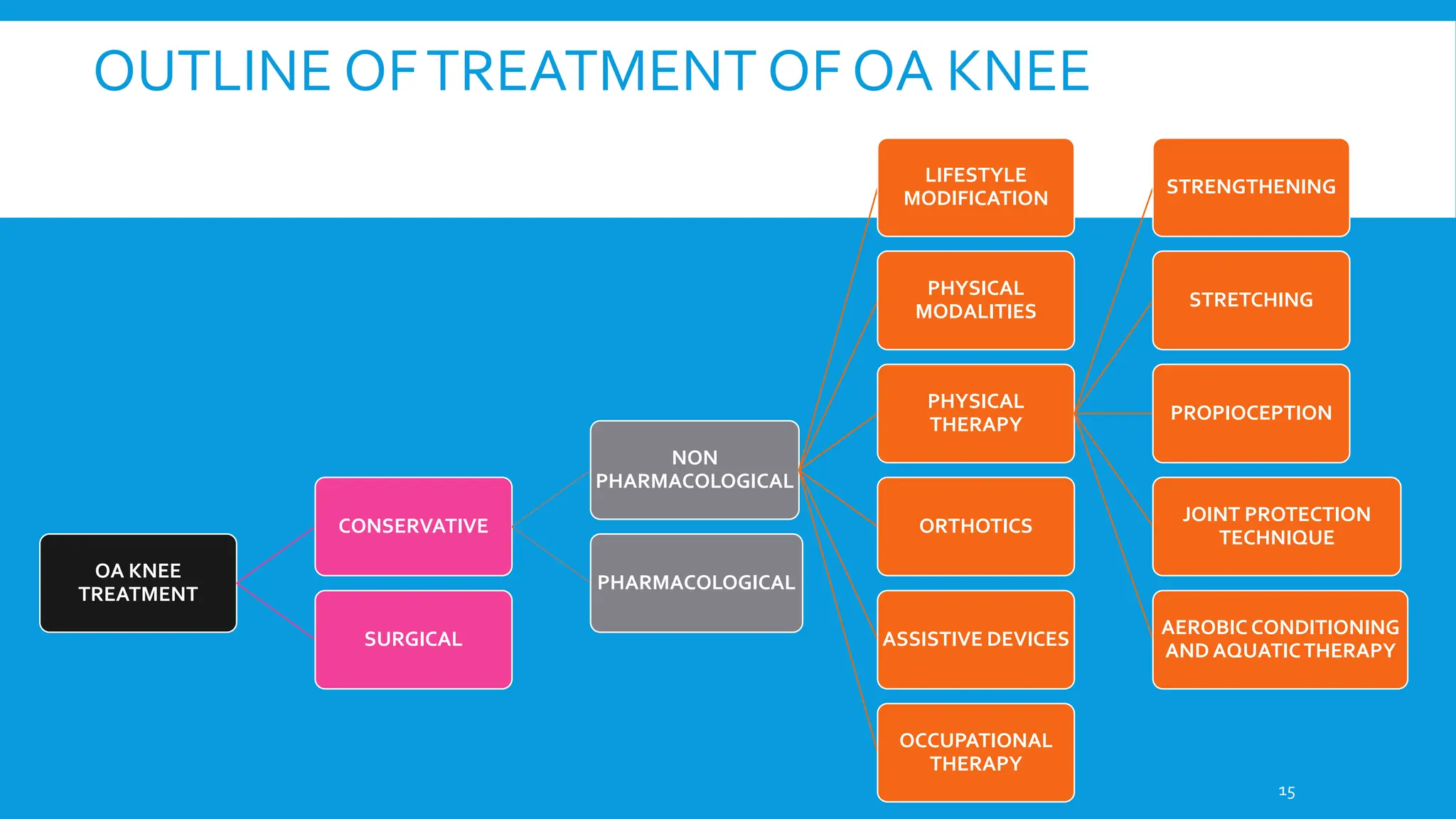
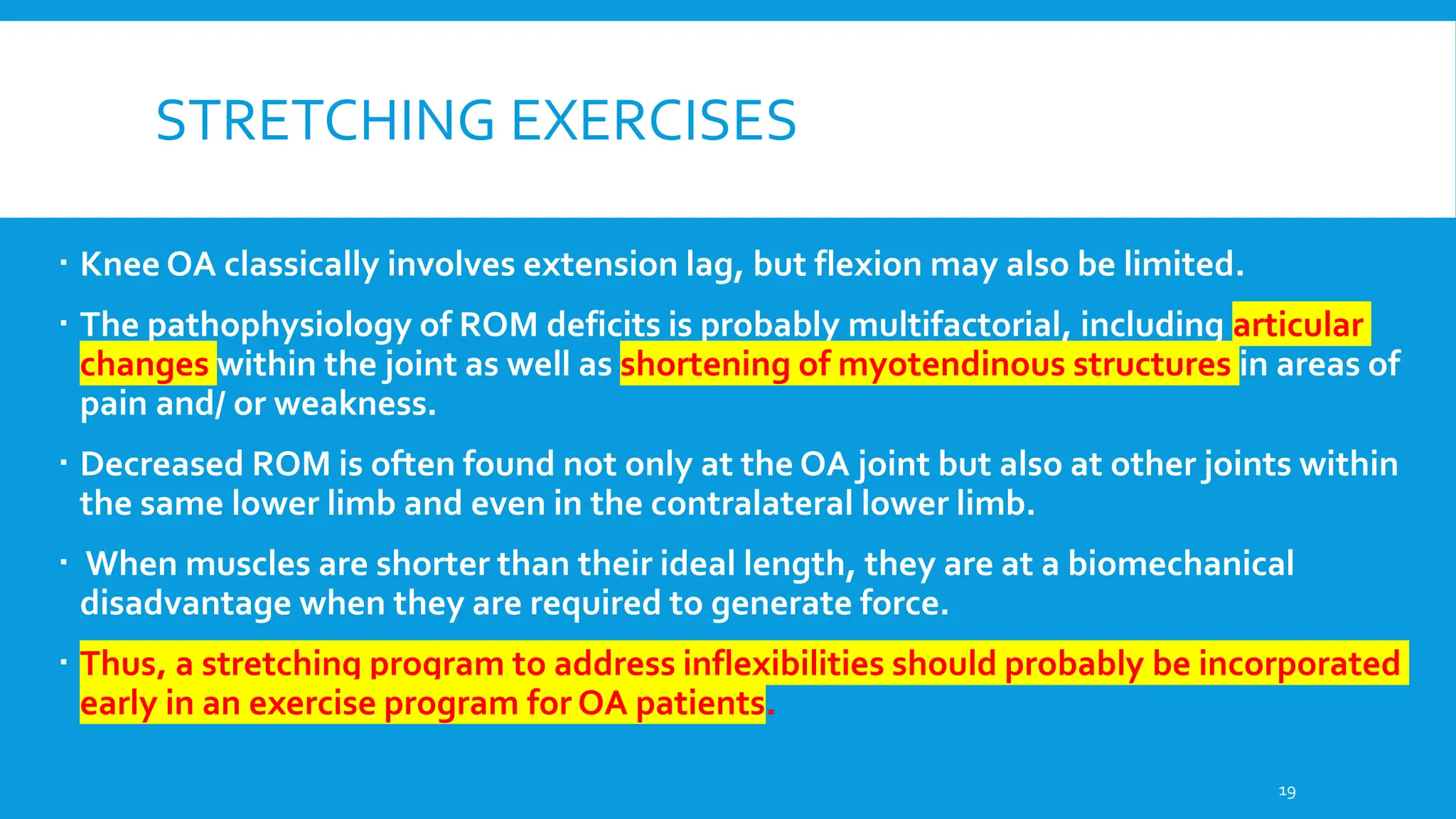
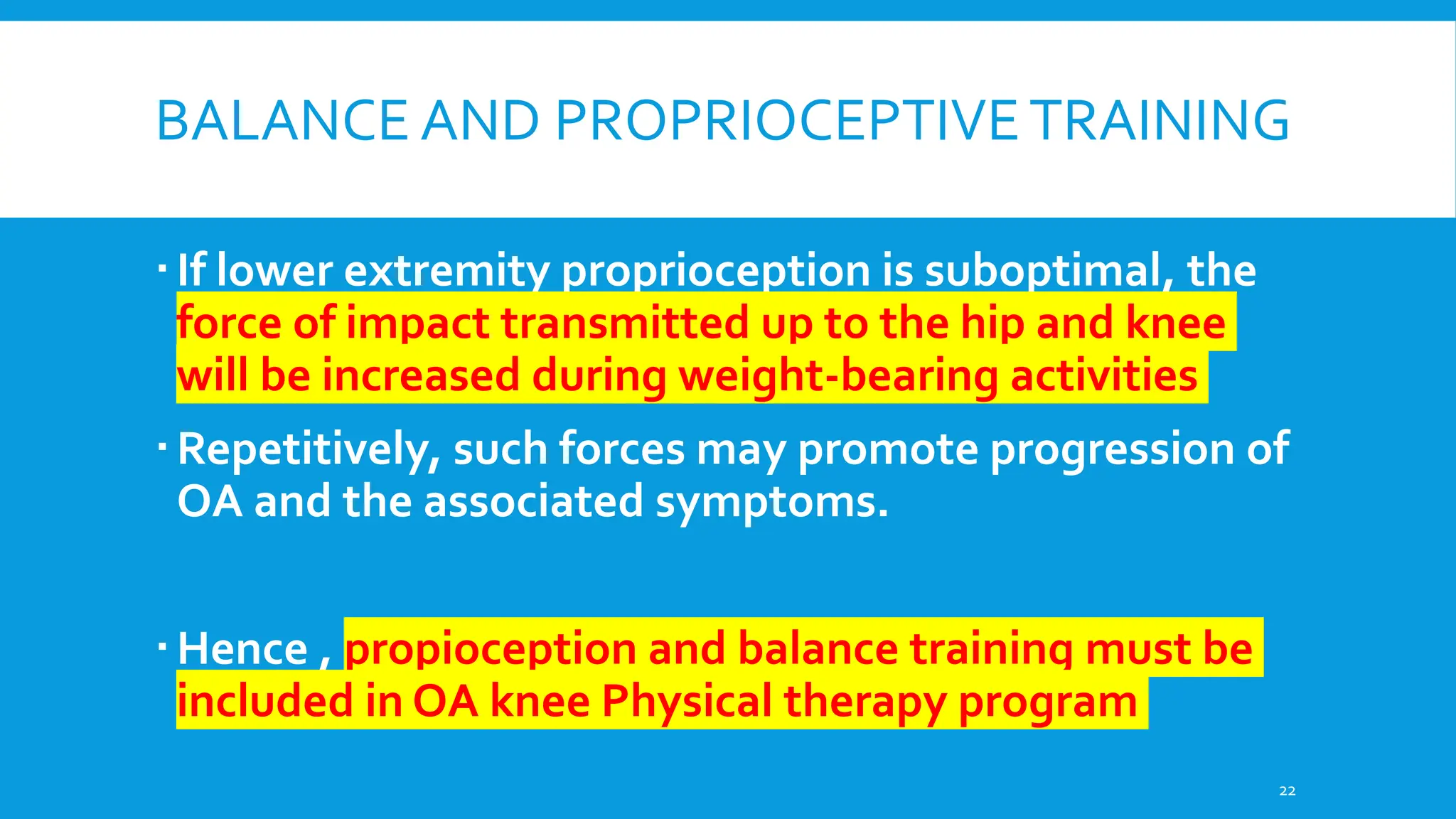
Osteoarthritis (OA) is a non-inflammatory, progressive joint disorder, commonly affecting the knee and hip, with a prevalence of 28.7% in India. Symptoms include dull aching pain, joint stiffness, and crepitus, while treatment focuses on non-pharmacological methods such as weight loss, physical therapy, and the use of orthotics. The document also discusses the radiological approach to OA diagnosis and outlines various management strategies.