1) A transfemoral amputation is the amputation of the lower limb between the hip joint and knee joint, commonly referred to as an above-knee amputation.
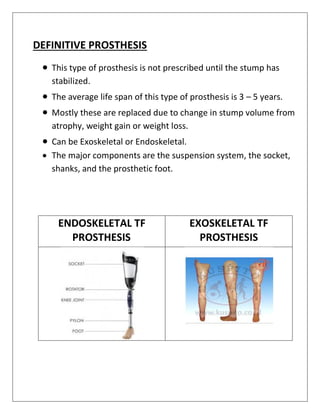
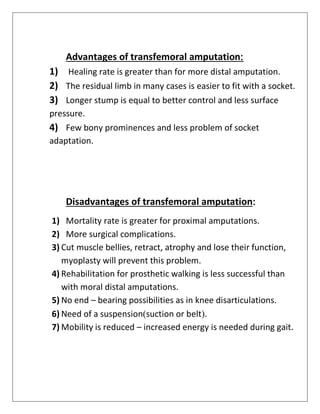
2) The ideal prosthetic management of a transfemoral amputation involves fitting the patient with a series of prostheses over time as the residual limb heals, including an immediate post-op prosthesis, initial prosthesis, preparatory prosthesis, and definitive prosthesis.
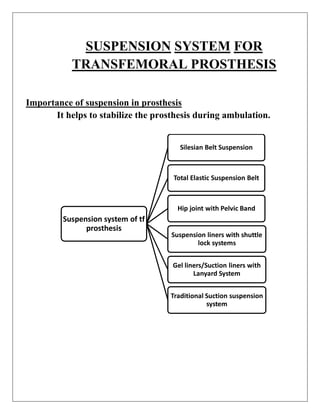
3) Transfemoral prostheses can use different suspension systems to secure the prosthesis to the residual limb, including belts, liners, suction, and locking mechanisms, with tradeoffs between functionality, comfort, and difficulty of use.
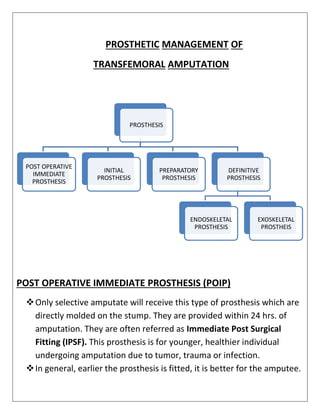
![INITIAL PROSTHESIS
▪ It is provided as soon as the sutures are removed.
▪ It is sometime referred to as Early Post Surgical Fitting (EPSF).]
▪ This can be prescribed after 4 weeks of amputation.
▪ Generally, EPSF is directly molded on the stump by pop bandage
or fiber glass bandage.
▪ This prosthesis is prescribed to prevent the patient’s muscles goes
into atrophy.
PREPARATORY PROSTHESIS
• It is referred to as temporary prosthesis.
• A temporary or preparatory prosthesis is used for weeks or
months until the stump has stabilized before the permanent or
definitive prosthesis is provided.
• The socket may made of either POP or a plastic material.
• The temporary prosthesis is endoskeletal and cannot be
exoskeletal.](https://image.slidesharecdn.com/prostheticscience1-240113191825-4ec810b2/85/Transfemoral-Prosthesis-Suspension-Socket-Design-5-320.jpg)