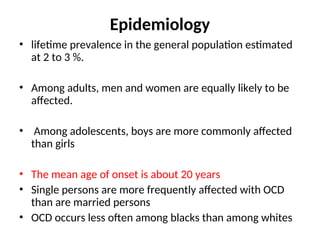
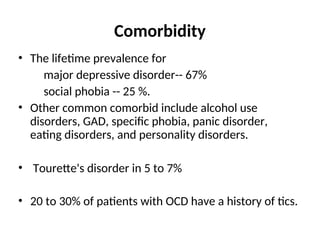
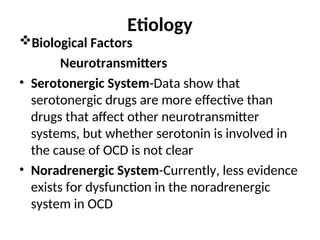
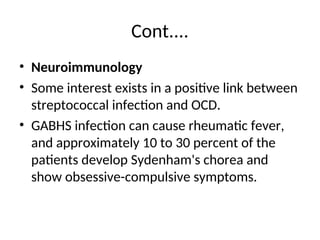
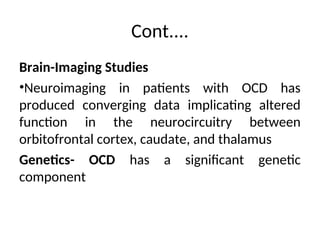
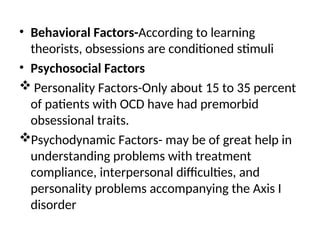
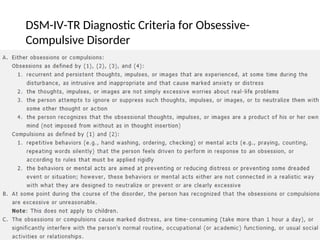
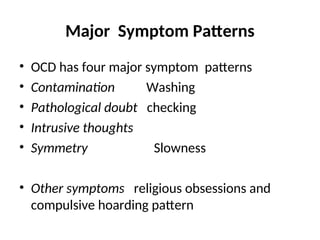
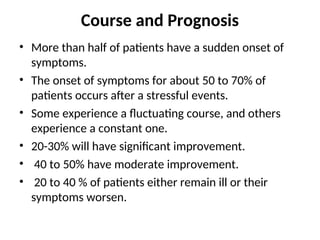
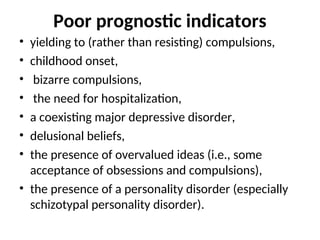
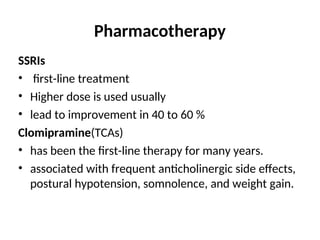
The document provides an overview of obsessive-compulsive disorder (OCD), including its definitions, epidemiology, comorbidity, etiology, diagnosis, and treatment options. It discusses key characteristics such as obsessions and compulsions, as well as statistical data on prevalence and associated disorders. Treatment options include pharmacotherapy, such as SSRIs and clomipramine, and behavioral therapies like exposure and response prevention, with an emphasis on the need for individualized approaches.