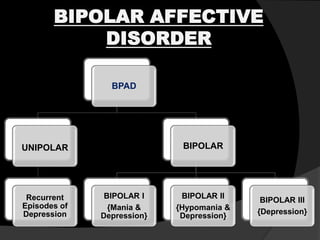
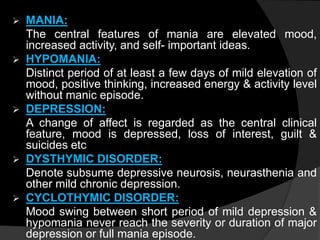
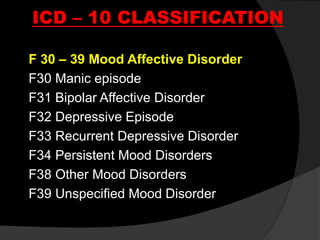
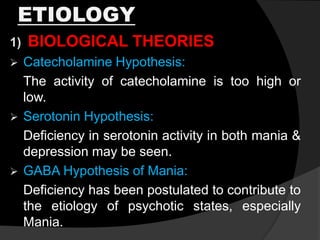
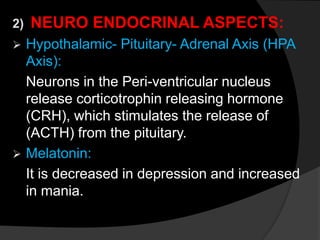
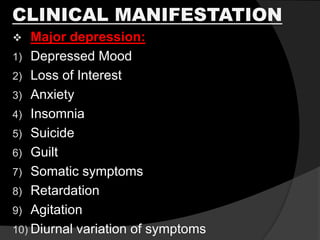
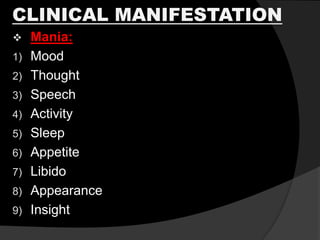
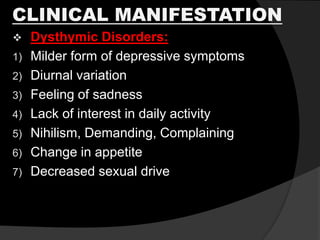
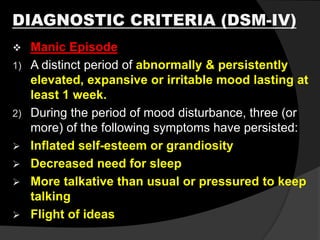
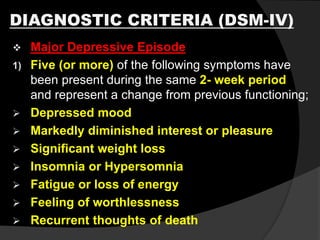
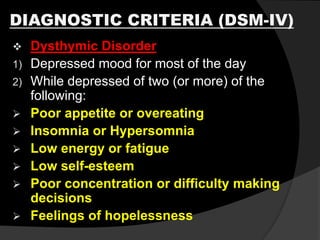
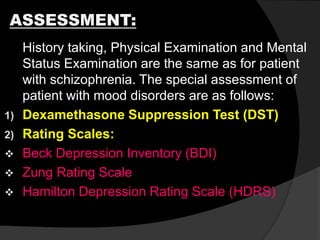
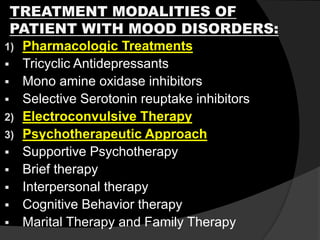
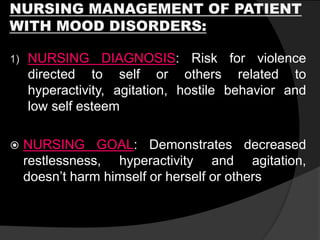
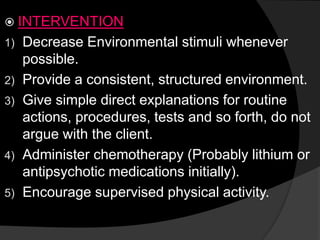
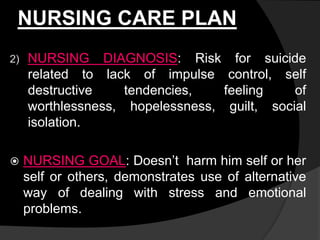
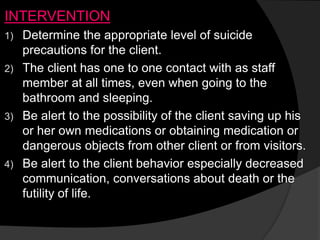
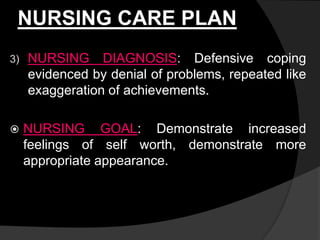
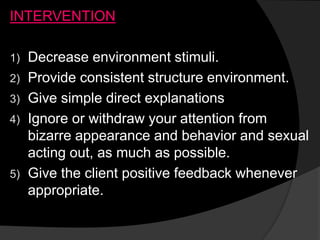
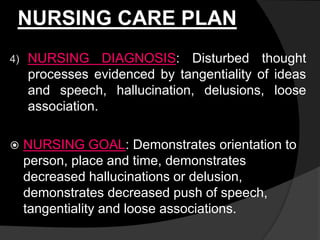
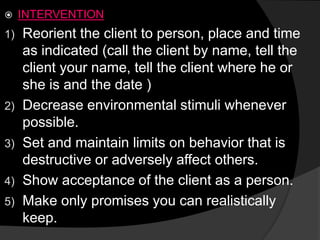
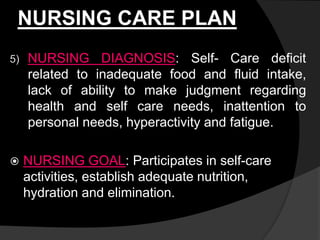
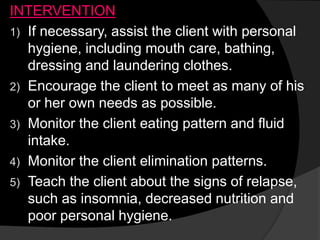
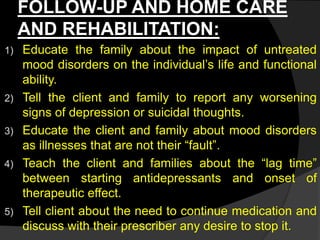
Mood disorders involve disturbances in mood that are accompanied by related cognitive, physical, and interpersonal difficulties. They include conditions like bipolar disorder and major depressive disorder. Bipolar disorder involves episodes of mania and depression, while major depressive disorder involves recurrent episodes of depression without mania. Mood disorders have biological, genetic, neurological, and psychosocial causes. They are diagnosed based on symptoms and treated with medications, psychotherapy, and electroconvulsive therapy with the goal of managing mood disturbances and related issues. Nursing care focuses on safety, treatment adherence, symptom monitoring, and education.