1) Obsessive Compulsive Disorder (OCD) is an anxiety disorder characterized by recurrent obsessions and/or compulsions that are time-consuming and cause distress or impairment.
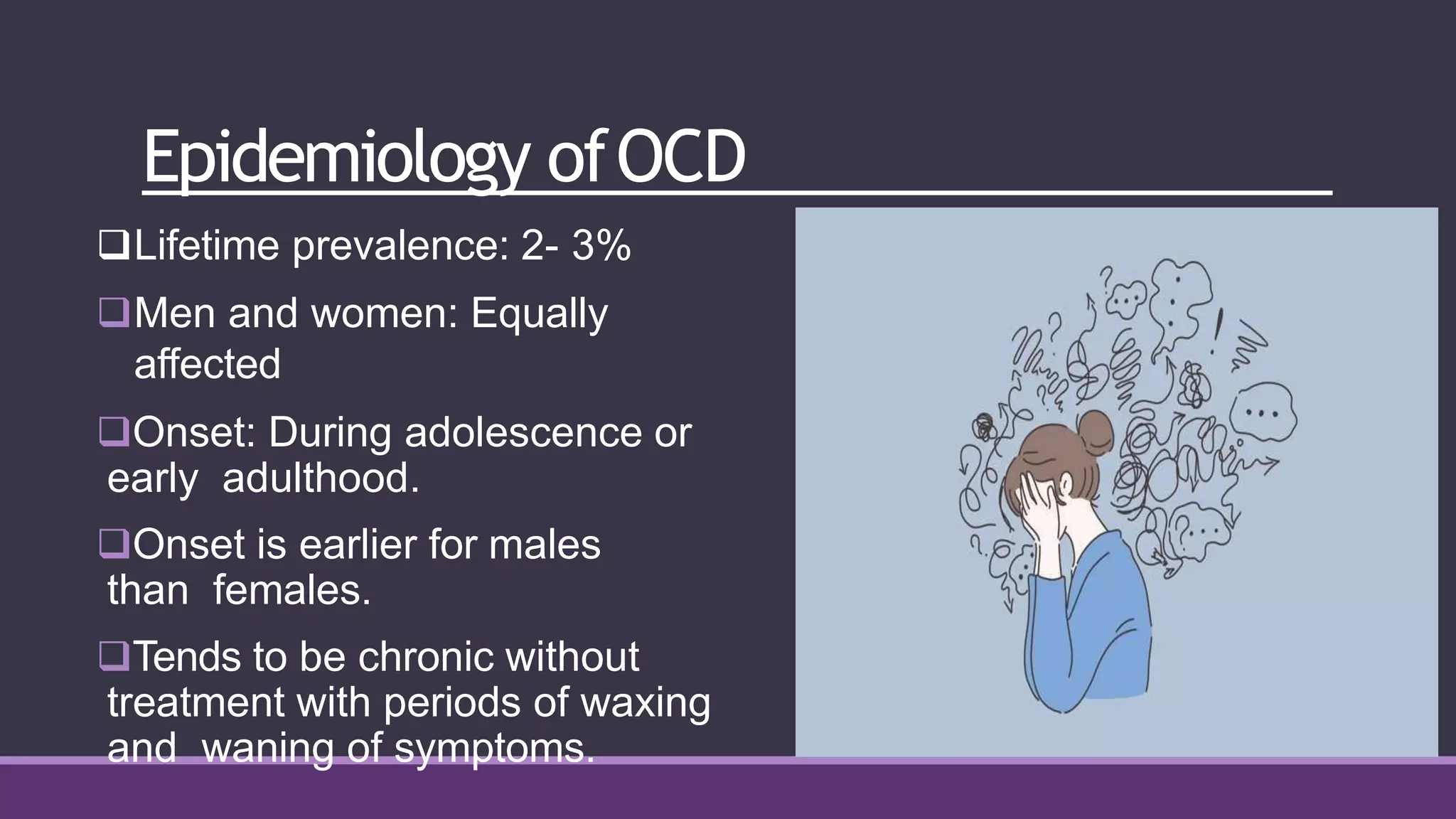
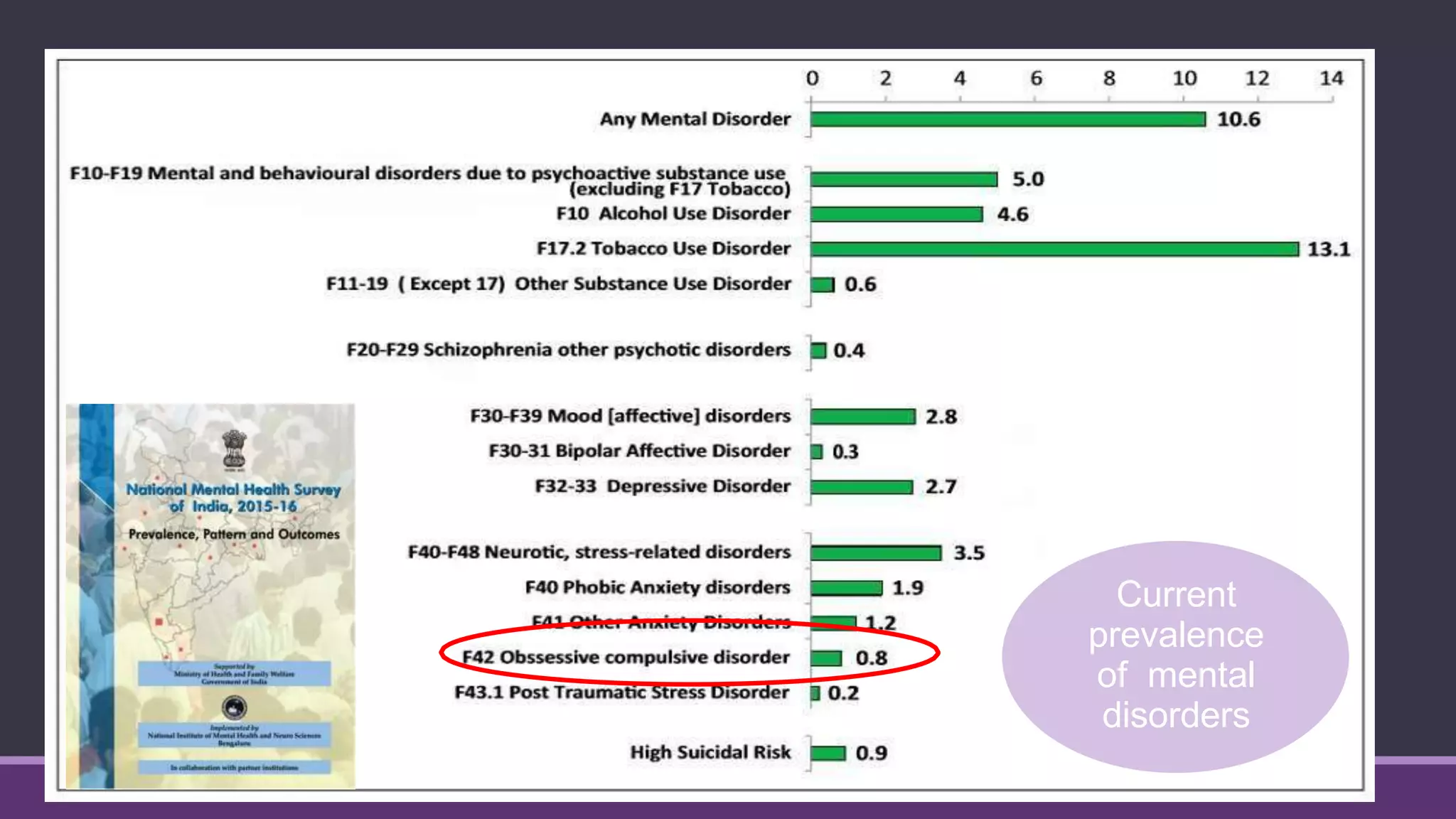
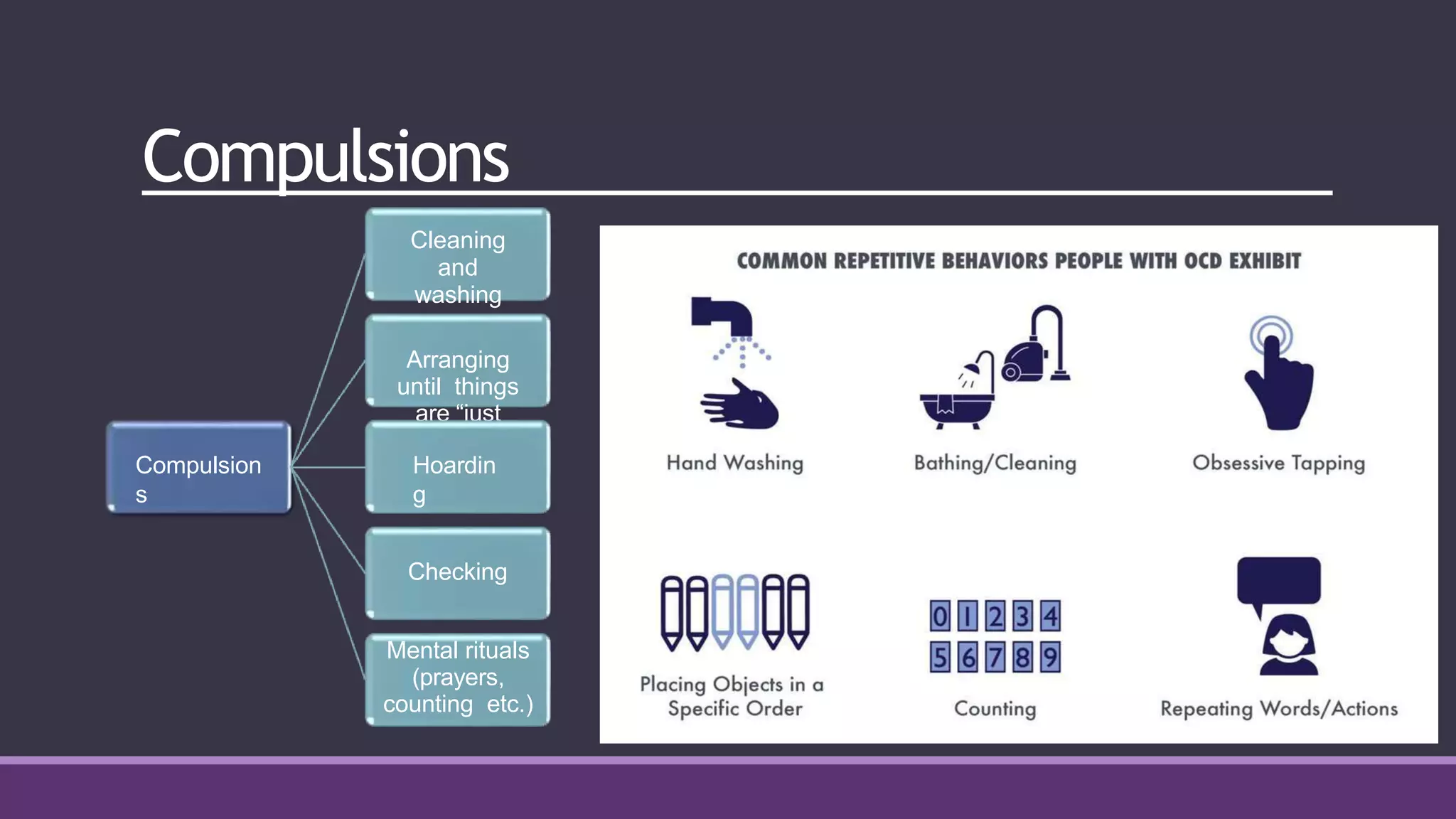
2) The lifetime prevalence of OCD is estimated to be 2-3% and it often begins during adolescence or early adulthood. Symptoms tend to be chronic without treatment and include obsessions about contamination, doubts, or intrusive thoughts paired with compulsive behaviors like cleaning, checking, or rituals.
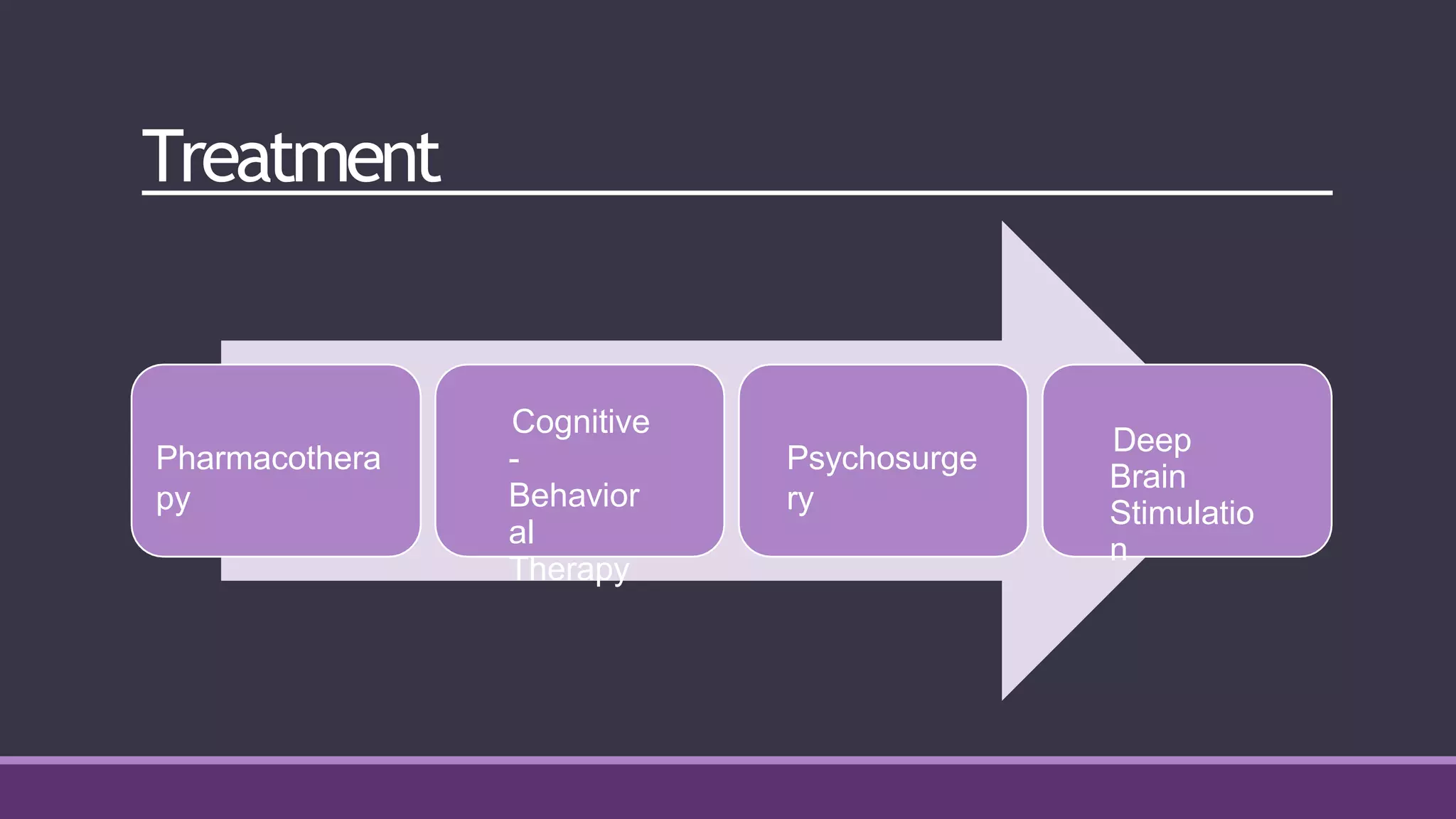
3) Cognitive-behavioral therapy (CBT), specifically exposure and response prevention (ERP), is the most effective treatment for OCD alongside selective serotonin reuptake inhibitor (SSRI) medications. CBT aims to challenge