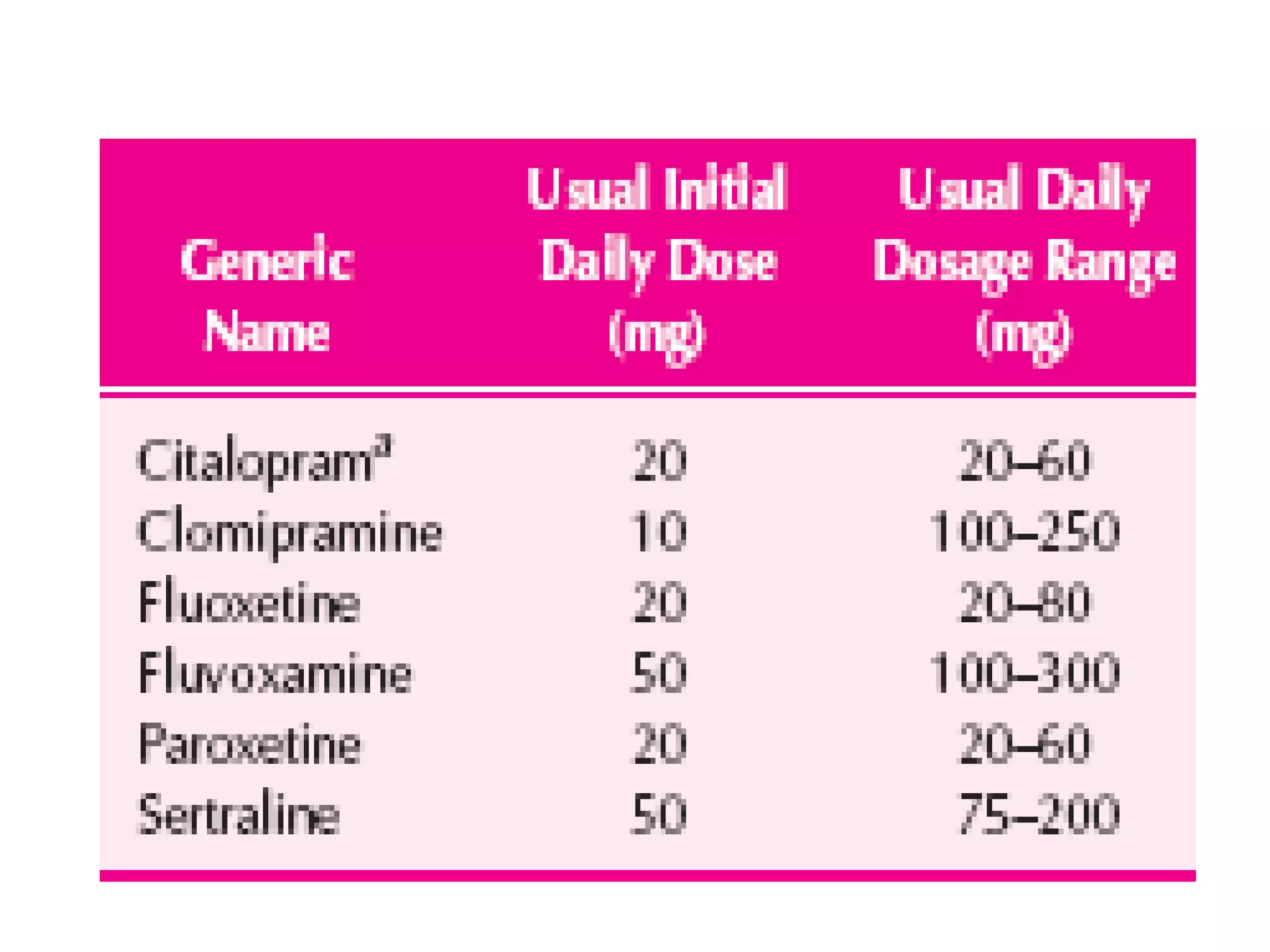
The document discusses obsessive compulsive disorder (OCD), detailing its diagnostic criteria from DSM-IV, where individuals must experience obsessions and/or compulsions that are time-consuming or cause significant distress. It describes common obsessions, compulsions, prevalence rates, and associated comorbidities, as well as diagnosis and treatment options such as cognitive behavioral therapy and medications. Additionally, it highlights the effectiveness of various drugs, potential side effects, and recommendations for treatment during pregnancy.