The document discusses schizophrenia, including its characteristic symptoms, subtypes, treatments, and theories about its causes. Some key points include:
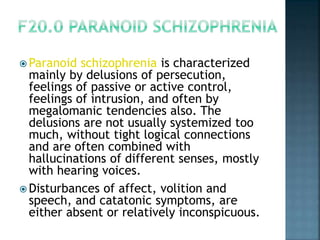
- The main symptoms of schizophrenia are delusions, hallucinations, and disorganized speech.
- There are several subtypes of schizophrenia including paranoid, catatonic, and undifferentiated.
- Both older "conventional" and newer "atypical" antipsychotic medications are used to treat schizophrenia by reducing positive symptoms.
- The dopamine hypothesis suggests psychotic symptoms are related to excess dopamine activity in the brain, which newer theories have expanded on to include other neurotransmitters.